Table of Contents
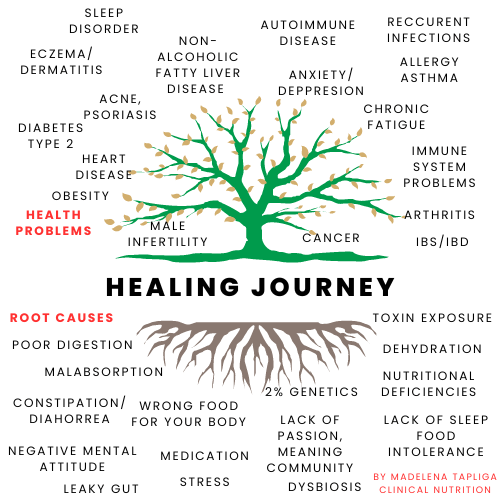
The liver is the most overworked organ in the body, having to break down all the increasing toxins found in our environment and our food, performing various essential functions such as detoxification and metabolism regulation. However, the liver can be affected by various diseases and conditions, such as fatty liver and cirrhosis.
Nonalcoholic fatty liver disease (NAFLD) is a common cause of chronic liver disease globally. It is often undiagnosed, even in advanced stages. NAFLD-cirrhosis is the most severe stage, with a high risk of hepatocellular carcinoma (HCC) and liver-related morbidity-mortality.
Fatty liver is a reversible condition in which fat builds up in the liver cells, usually due to excessive alcohol consumption and/or obesity.

Fast facts
If your liver is not functioning properly, toxins that would normaly be filtered by the liver will acumulate in the body. Most people’s lives work only at around 35-40% of their potential capacity, because of the large amount of toxins we ingest.
When its working properly, the liver can clean up to 99% of bacteria and toxins from the blood.
Around 2.25 litres (4 pints) of blood pass through the liver every minute for detoxification, and every day the liver manufactures about 1 litre (2 pints) of bile, which help carry away toxins via the bowel.
Due to the widespread epidemic of obesity and metabolic syndrome, NAFLD has emerged as the leading cause of chronic liver disease globally.
- Non-alcoholic fatty liver disease (NAFLD) affects 25% of the global population and can lead to cirrhosis and hepatocellular carcinoma.
- NAFLD includes a spectrum from simple fatty liver to non-alcoholic steatohepatitis (NASH), characterized by inflammation and faster fibrosis progression.
- There is a bidirectional association between NAFLD and metabolic syndrome, with type 2 diabetes increasing the risk of cirrhosis and complications.
- Cardiovascular disease and extrahepatic malignancy are leading causes of death in NAFLD patients, but advanced liver fibrosis is a key prognostic marker.
- Non-invasive tests can assess liver fibrosis, and patients with cirrhosis should be screened for hepatocellular carcinoma and oesophageal varices.
- Currently, there is no approved therapy for NAFLD, but several drugs are in advanced stages of development.
- Due to the complex pathophysiology and heterogeneity, combination treatments may be needed for many NAFLD patients.
- A healthy lifestyle and weight reduction are crucial for both the prevention and treatment of NAFLD.
The presence of cirrhosis in nonalcoholic-fatty-liver-disease (NAFLD) is the most important predictor of liver-related mortality.
Cirrhosis is a more severe and irreversible form of liver disease, characterized by scarring and reduced liver function.
These two conditions have some overlapping symptoms, such as fatigue, jaundice, and abdominal pain, but cirrhosis symptoms tend to be more severe and debilitating.
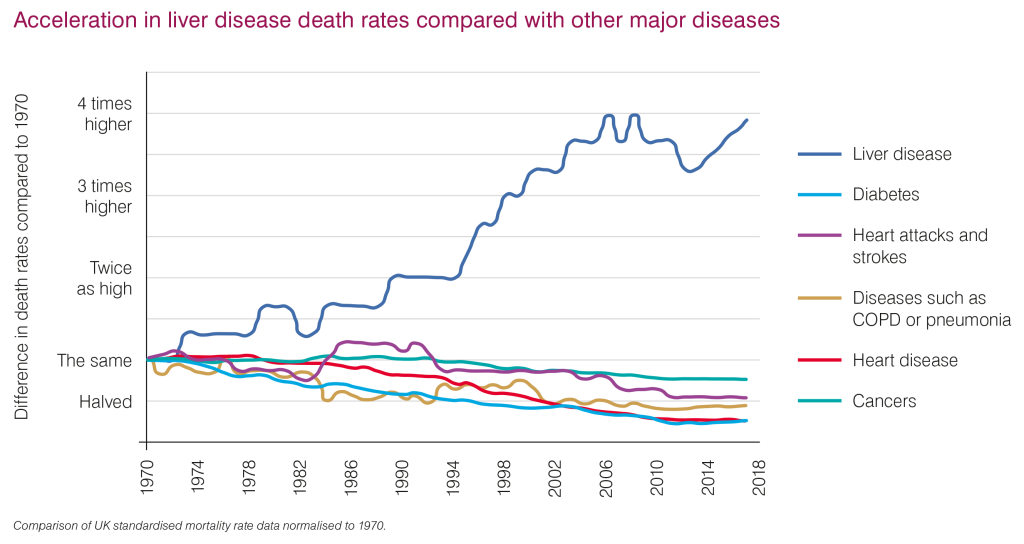
Did you know that liver disease is responsible for 2 million deaths worldwide?
1 in 3 liver deaths occur among females, making it the 11th leading cause of death globally and the 15th leading cause of disability-associated life-years.
Cirrhosis is an expensive disease
The economic burden of liver disease in the United States (2016) amounted to $32.5 billion.ks 15th in terms of disability-adjusted life-years
Exploring Liver Disease: Essential Facts and Statistical Insights
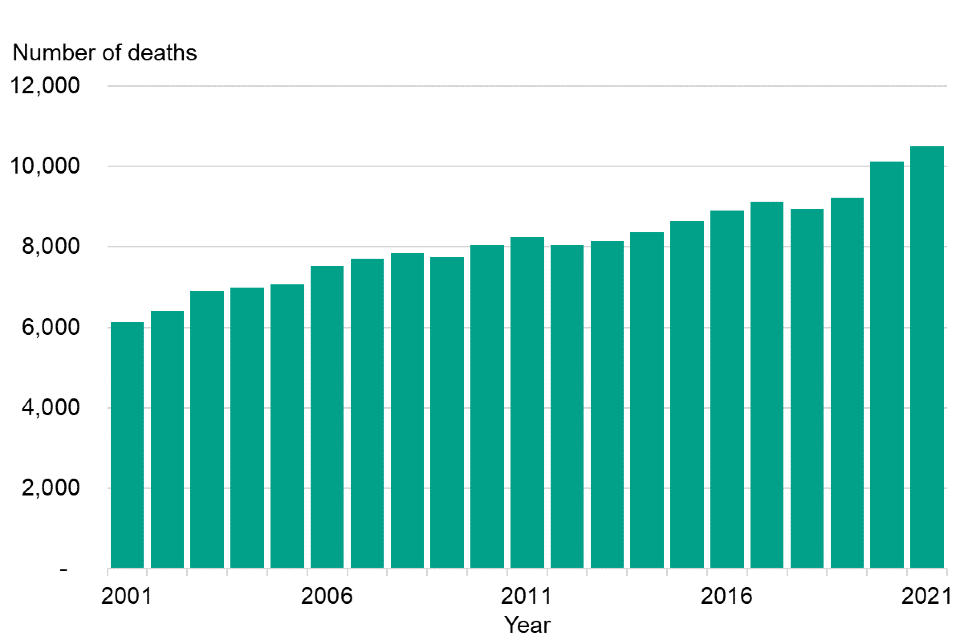
The number of deaths caused by liver disease in people under the age of 75 in England, from 2001 to 2021.
The progression of fatty liver to cirrhosis may take many years, and not every individual with fatty liver will develop cirrhosis. The speed at which this progression occurs depends on the underlying causes and the individual’s overall health. The difference between fatty liver and cirrhosis, as well as the effectiveness of various treatments, can be determined through diagnostic techniques, such as ultrasound imaging, blood tests, and liver biopsy. Both conditions can benefit from lifestyle modifications, like adopting a healthy diet and abstaining from alcohol, but more advanced treatments and medical interventions may be necessary for cirrhosis.
Fatty Liver Causes
Fatty liver, also known as hepatic steatosis, is a condition where excess fat accumulates in the liver. This can lead to inflammation, liver damage, and eventually, cirrhosis. The main causes of fatty liver include obesity, high blood sugar, insulin resistance, and high levels of triglycerides in the blood.
There are two types of fatty liver: nonalcoholic fatty liver disease (NAFLD) and alcoholic fatty liver disease (AFLD). NAFLD is not caused by alcohol consumption, but rather by metabolic syndrome, whereas AFLD is a result of excessive alcohol intake. Both conditions can progress to more severe liver diseases like cirrhosis or liver cancer.
Patients with non-alcoholic fatty liver disease have exhibited reduced levels of serum zinc, copper, vitamins A, C, D, E, and carotenoids. Additionally, an excess of iron and selenium has been implicated in the severity of NAFLD.
A common risk factor for fatty liver is an unhealthy diet, which can include high-fat and high-sugar foods. Additionally, a sedentary lifestyle and genetics can also play a role in the development of fatty liver.

Fatty Liver Diagnosis
Diagnosing fatty liver usually involves a combination of tests and medical exams.
In the early stages of NAFLD, most patients do not experience symptoms. However, some may experience discomfort in the upper right quadrant and general fatigue. During a physical examination, hepatomegaly and tenderness in the upper right quadrant may be observed. NASH refers to the histologic changes in the liver, characterized by hepatic steatosis, inflammation, and hepatocellular damage, unrelated to excessive alcohol consumption. Reporting accurate information about alcohol consumption is necessary for NAFLD/NASH diagnosis.
Blood tests to detect any liver enzyme abnormalities ( ALT, AST, ALP, GGT, albumin, prothrombin time (PT), Cytokines and Inflammation Biomarkers, Oxidative Stress Markers, Noninvasive Serum Biomarkers of Fibrosis, Potential Genetic Modifiers and Novel Markers
Imaging tests like ultrasound, CT scan, or MRI can detect fat accumulation in the liver. However, an ultrasound may not be able to differentiate between fatty liver and cirrhosis.
A liver biopsy is the gold standard for diagnosing fatty liver and assess the extent of liver damage.
Can fatty liver or cirrhosis be identified without a doctor’s visit?
It’s highly unlikely. While some symptoms may suggest liver issues, such as fatigue, weight loss, or abdominal pain, these signs are not specific to fatty liver or cirrhosis. Only a doctor can provide an accurate diagnosis through a thorough examination and medical tests.
Overview of Cirrhosis
Cirrhosis’s clinical manifestations have been recognized since ancient times. The Ebers papyrus, dating back to around 2600 BC, describes ascites, linking it to a “hardness of the liver” and excessive alcohol intake. Decompensated cirrhosis manifests through evident signs such as abdominal swelling, jaundice, and gastrointestinal bleeding.
Cirrhosis is a late-stage liver disease characterized by the scarring of liver tissue due to long-term damage, impairing the liver’s ability to regenerate and function properly. Common causes include chronic alcohol abuse, hepatitis B and C, and non-alcoholic fatty liver disease.

Stages and Progression of Cirrhosis
Cirrhosis progresses in four stages:
- Compensated cirrhosis: The liver is functioning, but there is potential for further damage. At this stage, a person may not experience symptoms.
- Decompensated cirrhosis: The liver loses its ability to compensate for damage, and symptoms begin to appear. These can include jaundice, fatigue, and fluid buildup in the abdomen (ascites).
- End-stage liver disease (ESLD): Severe complications arise, such as bleeding in the gastrointestinal tract, infections, and kidney dysfunction.
- Liver failure: The liver loses its ability to function, and a liver transplant is required.
The progression of cirrhosis varies depending on the individual and the underlying causes. In some cases, it may take several years for a fatty liver to advance to cirrhosis.
Can an Ultrasound tell the difference between fatty liver and cirrhosis?
Diagnosing Cirrhosis
Cirrhosis is initially detected through blood tests, followed by imaging studies such as ultrasound, CT scan, or MRI. A liver biopsy can confirm the diagnosis, as histological examination allows medical professionals to assess the extent of liver scarring and damage.
There are non-invasive methods to differentiate between fatty liver and cirrhosis. For example, ultrasound can detect the textural differences between a fatty liver, which has a bright echogenic appearance, and a cirrhotic liver, which may exhibit a heterogeneous or coarse pattern.
It uses high-frequency sound waves to create images of the liver’s structure and texture, thus enabling doctors to identify any abnormalities.
On an ultrasound, a fatty liver typically appears as a brighter image compared to the normal liver tissue. This is due to the increased reflection of sound waves caused by the excess fat.
An early diagnosis of cirrhosis is crucial to managing the condition.
Cirrhosis is a more advanced stage of liver disease characterized by the replacement of healthy liver tissue with scar tissue. This occurs as a result of long-term liver damage. In an ultrasound, cirrhosis generally presents as a shrunken and irregular liver with an uneven surface, and the blood flow in the liver may also be altered.
Though ultrasound can provide a wealth of information about the liver’s condition, it is essential to understand that this imaging technique has its limitations. While it can help detect fatty liver and cirrhosis, differentiating between the two conditions solely based on ultrasound images may be challenging, particularly in the early stages. In some cases, additional tests like liver function tests, blood tests, or liver biopsies may be required for a more accurate diagnosis.
Bioresonance therapy is an alternative or complementary medicine approach that involves measuring electromagnetic waves emitted by the body and using them to diagnose and treat various health conditions.
What is the Difference between Fatty Liver and Cirrhosis?
Fatty liver, also known as steatosis, is a condition where excess fat accumulates in the liver. In most cases, fatty liver does not cause any symptoms, and individuals might not even realize they have it. However, some people may experience fatigue, abdominal discomfort, and unexplained weight loss.
On the other hand, cirrhosis is a severe form of liver disease characterized by the formation of scar tissue in the liver. The symptoms of cirrhosis can be more pronounced than those of fatty liver, including jaundice (yellowing of the skin and eyes), fluid accumulation in the abdomen (ascites), easy bruising, and mental confusion.
How Fatty Liver Leads to Cirrhosis
Fatty liver can progress to a more severe form called non-alcoholic steatohepatitis (NASH), where the liver becomes inflamed and damaged. If left untreated, NASH can eventually lead to cirrhosis, causing extensive liver damage and reduced function. This progression is due to the continuous accumulation of fat and inflammation, which results in the formation of scar tissue, impairing the liver’s ability to function properly.
It is essential to note that not all cases of fatty liver develop into cirrhosis. Factors like obesity, diabetes, and high blood pressure increase the risk of progression. Maintaining a healthy lifestyle by following a balanced diet, exercising regularly, and maintaining a healthy weight can help prevent and reverse fatty liver before it progresses to more severe liver damage.
Fatty Liver and Cirrhosis Diet
Changing your diet and being physically active are still the main ways to address this issue. Studies show that eating healthy and losing weight early on in Non-Alcoholic Fatty Liver Disease (NAFLD) can help control its progression.
Managing the cause of liver damage, such as reducing alcohol consumption or treating viral hepatitis, can help prevent the progression of cirrhosis and improve liver function. A well-balanced diet, guided by a physician or dietician, is recommended for those with liver diseases like fatty liver and cirrhosis.
How to reduce fatty liver?
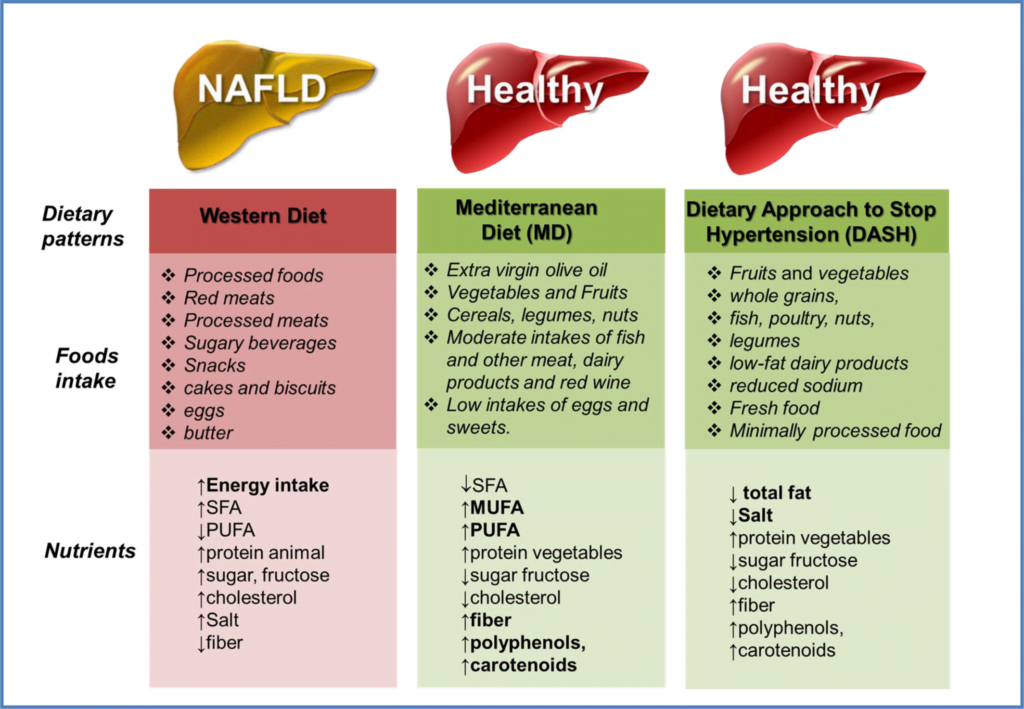
When aiming to manage fatty liver or cirrhosis, it is essential to make dietary adjustments. For a healthy liver, it is crucial to avoid foods high in unhealthy fats, sugar, and sodium, while incorporating nutrient-dense options. Foods to avoid include:
- Fried or processed foods
- Avoid eating excessive proteins
- Foods high in saturated fats
- Sugary drinks and snacks, fructose
- Melted cheese is very difficult for the liver to process. Pizza should be avoided as well.
- Alcohol, caffeine
- Eggs are an excellent source of protein, however, they are hard to digest if you have liver issues. Keep it down to two a week
- Avoid eating or drinking grapefruit.
Medication to avoid with fatty liver disease: paracetamol, aspirin, and most other medications place a strain on the liver.
Foods to include in your diet should be rich in antioxidants, fiber, and healthy fats. Some examples are:
- Fresh fruits and vegetables, especially those rich in antioxidants: organic carrots, sweet potato, pumpkin, papaya, mangoes, alfalfa, and watercress
- eat more beetroot, raw or cooked- it’s one of the best vegetables for the liver because it helps digestion, improves liver function, and reduces constipation
- Whole grains
- Lean proteins
- Omega-3 fatty acids (found in fish)
- Vitamin E supplementation is a prevalent practice among patients with non-alcoholic fatty liver disease (NAFLD).
A new approach, called ‘nutritional geometry’ considers the importance of integrating nutrition, animals and the environment.

Medical Interventions and Treatments
Management of chronic liver disease involves counseling, laboratory testing, and ultrasound monitoring.
Treatment goals: prevent cirrhosis, decompensation, and death. Varices monitored with endoscopy, often require nonselective beta blockers.
Ascites treatment includes diuresis, salt restriction, and antibiotic prophylaxis for spontaneous bacterial peritonitis.
Hepatic encephalopathy is effectively managed through lifestyle and nutritional modifications, supplemented with lactulose and rifaximin as necessary.
Regular ultrasound screening every six months is recommended for cirrhotic patients to detect hepatocellular carcinoma.
Treatments for Fatty Liver
- Weight Loss: Losing weight can help reduce fat accumulation in the liver and improve liver function.
- Diabetes Management: Patients with diabetes should work closely with their healthcare professionals to control blood sugar levels, which can help prevent fatty liver development.
- Alcohol Consumption: Reducing or eliminating alcohol intake can significantly improve liver health.
- Medications: In some cases, doctors might prescribe medications like betablockers, lactulose,and rifaximin and Vitamin E to treat fatty liver caused by non-alcoholic factors.
Managing Cirrhosis Medically
Cirrhosis, a more advanced liver disease involving scarring and impaired function, requires ongoing medical management. The following treatment options may be recommended for cirrhosis patients:
- Medication to Reduce Liver Inflammation: Doctors might prescribe corticosteroids to control inflammation and prevent further liver damage.
- Treatment of Liver Infections: Patients with viral hepatitis or other liver infections should undergo appropriate treatment to prevent further liver damage.
- Medications for Complications: Medications are often used to manage common complications of cirrhosis, such as ascites, portal hypertension, and encephalopathy.
- Liver Transplant: In severe cases, a liver transplant might be recommended when the liver is no longer functioning effectively.
Meal Ideas for Cirrhosis
Diet plays an important role in managing both fatty liver and cirrhosis. Patients with cirrhosis should focus on consuming well-balanced, nutrient-dense meals that promote liver health. Below is a list of dietary recommendations for cirrhosis patients:
- Protein: Include lean protein sources such as fish, poultry, and legumes in your meals to support liver repair.
- Fruits and Vegetables: Incorporate a variety of colorful fruits and vegetables, as they are rich in antioxidants and other nutrients that can fight liver inflammation.
- Whole Grains: Opt for whole-grain bread, pasta, and brown rice, as they provide essential nutrients and fiber for liver health.
- Low Sodium: Limit your daily sodium intake to help prevent fluid build-up in the abdomen and lower the risk of complications related to cirrhosis.
Can Fatty Liver Turn into Cirrhosis?
While not every fatty liver progresses to cirrhosis, the risk increases with ongoing factors such as alcohol abuse, obesity, and type 2 diabetes. If left untreated, fatty liver can lead to inflammation, liver cell damage, and eventually, cirrhosis.
To prevent the progression from fatty liver to cirrhosis, it is crucial to address the underlying causes. Lifestyle changes, such as adopting a healthy diet, regular exercise, and reducing alcohol intake, can help.
Reversibility of Fatty Liver and Cirrhosis
Fatty liver is a reversible condition if addressed early on. By implementing a balanced diet, focusing on whole grains, lean proteins, and plenty of fruits and vegetables, patients can reduce liver fat. Furthermore, incorporating regular exercise and maintaining a healthy weight can significantly improve liver function.
Cirrhosis, however, is often irreversible due to the advanced scarring and damage to liver tissue. Nonetheless, early detection and treatment can slow down the progression and ease symptoms. In severe cases, a liver transplant might be necessary.
- Fatty liver treatments:
- Weight loss
- Balanced diet
- Regular Exercise
- Limiting alcohol intake
- Cirrhosis treatments:
- Medications
- Monitoring for complications
- Liver transplant, if necessary
In conclusion, while fatty liver has the potential to progress to cirrhosis, early detection and immediate lifestyle changes can prevent this. Fatty liver is a reversible condition, whereas cirrhosis is often considered irreversible. Regular medical check-ups and addressing the underlying causes play a vital role in managing both conditions.
Herbal and Plant Remedies
Herbs and plants have been used for centuries to treat various health conditions, including liver diseases. Some popular herbal remedies for liver health include:
- Milk thistle: Milk thistle is well-known for its liver-protective effects. It contains a compound called silymarin, which has antioxidant and anti-inflammatory properties. Silymarin is believed to help improve liver function and detoxification processes.
- Turmeric: This yellow spice contains an active ingredient called curcumin, which has powerful anti-inflammatory and antioxidant properties. Curcumin has shown promising results in reducing liver inflammation and fibrosis in various studies2.
- Dandelion root: Dandelion root is a natural diuretic and has been traditionally used for liver detoxification. It is believed to help stimulate bile production and improve digestion
- Good quality multi vitamins/minerals
- DMSO a key nutrient needed by the liver is sulphur
- the most powerful antioxidant and detoxifying compound in the liver is glutathione.
- Try this Tea, Your Liver will Thank You!
It’s essential to consult with a healthcare professional before using any herbal or plant remedies, especially if you have existing liver conditions or are taking prescription medications.
Can Fatty Liver – Cirrhosis Be Reversed?
It’s important to note that while herbal remedies and dietary changes can help support liver health, cirrhosis is a more advanced stage of liver disease that may not be reversible. However, adopting a healthier lifestyle can prevent further complications and improve quality of life.
Conclusion
How long take for fatty liver to turn into cirrhosis?
The time it takes for fatty liver disease to progress to cirrhosis varies among individuals and depends on several factors, such as the underlying cause, lifestyle choices, and genetic predisposition. In cases of non-alcoholic fatty liver disease (NAFLD), it may take several years or even decades for cirrhosis to develop. However, with proper lifestyle changes and medical treatment, this progression can be slowed down or prevented.
How do you know if you have fatty liver or cirrhosis?
Changing your diet and being physically active are still the main ways to address this issue. Studies show that eating healthy and losing weight early on in Non-Alcoholic Fatty Liver Disease (NAFLD) can help control its progression. Fatty liver symptoms are generally mild and can include fatigue, abdominal discomfort, or a feeling of fullness in the right upper abdomen. Cirrhosis presents with more noticeable and severe symptoms, such as jaundice (yellowing of the skin and eyes), edema (swelling), easy bruising and bleeding, abdominal fluid accumulation, and mental confusion.
It is highly recommended to consult your General Practitioner for a thorough physical examination and additional investigations. Additionally, it would be beneficial to request nutritional support.
Over the past decade, there has been significant research into the connection between nutrients, dietary patterns, and NAFLD. Understanding the role of nutrition in managing patients with NAFLD poses a substantial challenge. This is important factor since lifestyle changes, encompassing diet, exercise, and weight loss, have proven effective in controlling NAFLD.
Foods rich in antioxidants and anti-inflammatory properties, such as fruits, vegetables, and whole grains, herbal remedies, good quality multivitamins, Vitamine E, DMSO, and glutathione can support liver function. Avoiding fatty, processed foods and excessive alcohol consumption is crucial for preventing the progression from fatty liver to cirrhosis.
It is essential to consult a healthcare professional for a comprehensive evaluation and appropriate treatment plan tailored to individual circumstances.
Looking to the Future: The Role of Personalized Nutrition! 🙂
Hello readers! Thank you for taking the time to read our content. We hope you found it informative and engaging. We would love to hear your thoughts and opinions on the topic discussed. We also invite you to ask any questions that may have come up while reading.
Our team is more than happy to answer any queries you may have.
Hence, don’t hesitate to reach out and start a conversation with us!
We look forward to hearing from you 🙂
+0
Happy and healthy clients!
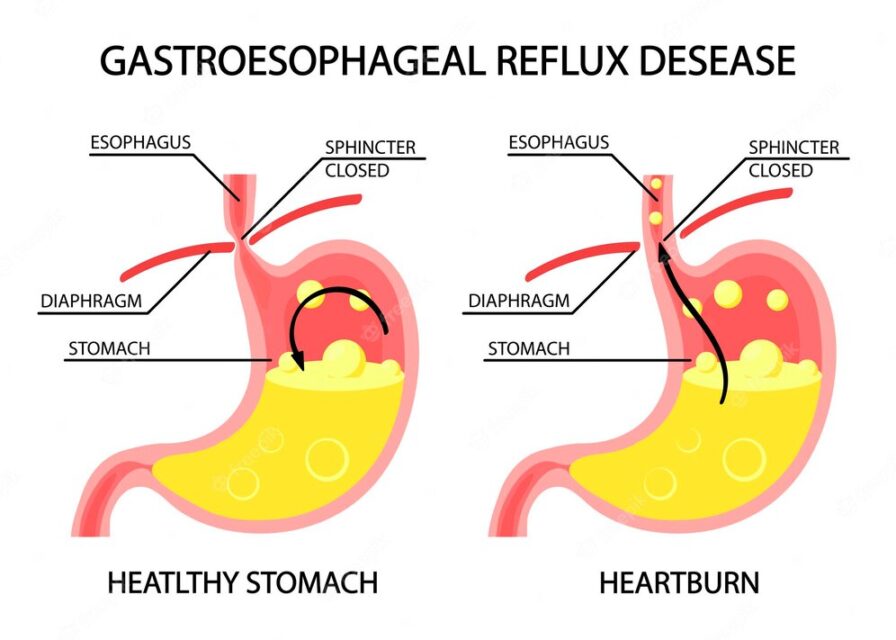
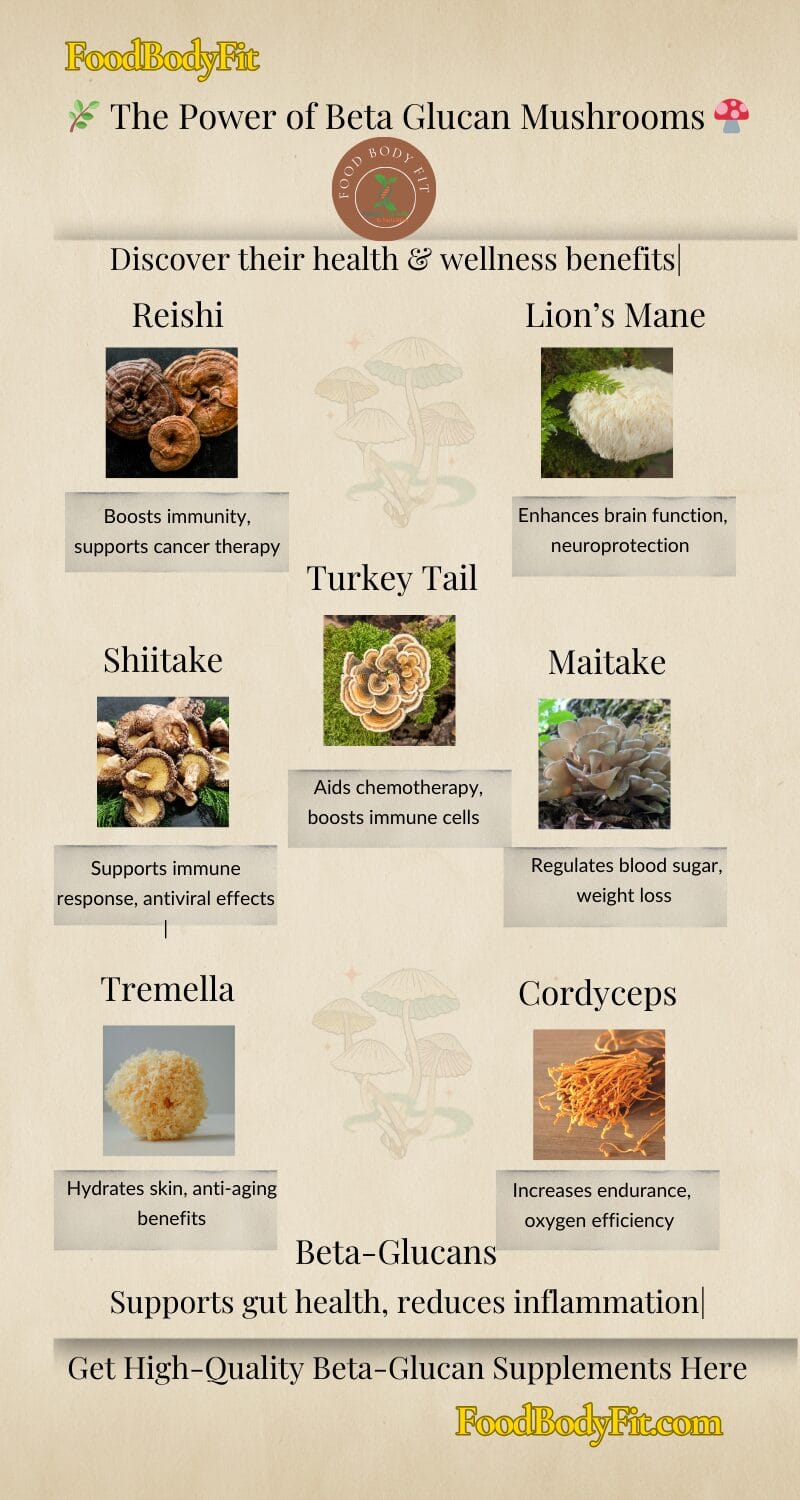
Which Mushroom Is Best For Gut Health? Unlock The Secret
Do you suffer from Gastro-esophageal reflux disease (GERD) ?Is mushroom bad for GERD?Are mushrooms good for GERD?Are reishi mushrooms…
Forgotten Superfood Turkey Tail Mushroom, Will Change Your Life Forever
Table of ContentsTurkey Tail Mushroom Medicinal Uses, Benefits, and Side Effects Explained: Coriolus Versicolor InsightsKey TakeawaysMechanisms of Action of…
Amazing Elixir of Life-Best Medicinal Mushroom Powder UK
Experience Wellness – The Elixir of Life AwaitsBest Medicinal Mushroom Powder: Medicinal Fungi, Your Forest FriendsMedicinal Mushrooms and connection to…
Is Diabetes A Nutritional Deficiency Disease: 8 Missing Important Nutrients
Type 2 Diabetes Nutritional Deficiency: Exploring Causes, Supplements, and Prevention StrategiesIs Diabetes A Nutritional Deficiency Disease?Causes and Risk FactorsThe…
10 Best Medicinal Mushrooms and Diabetes Management
People are going to start realizing, why take those antibiotics that are extracts of mushrooms? Why not just have…
5 Hidden Secrets of Maitake mushroom and Weight Loss
Which mushroom helps with weight loss?Grifola frondosa Dancing Mushroom OverviewMaitake mushroom nutrition factsHealth Benefits of Maitake mushroomImmune System SupportCancerCardiovascular…
Can Lion’s Mane Help With ADHD?
Table of ContentsBenefits of Lion’s Mane on Brain Function: A Comprehensive Guide to Benefits, Dosage, and NutritionDoes Lion’s Mane…
Secrets of Mind-Blowing Cordyceps Mushrooms And Female Fertility
Cordyceps Mushrooms and Female Fertility: Unveiling Natural Benefits for Enhancing Reproductive HealthOverview of Cordyceps Mushroom benefitsHistorical UseModern ApplicationsCordyceps For Female…
The Best Tremella Mushroom Guide: 11 Amazing Health Benefits Of
What is tremella mushroom good for?Why History MattersTremella Mushroom Nutrition FactsVitamins and MineralsMacronutrients Tremella Mushroom Health BenefitsCreates Youthful Healthy…
Fatty Liver and Cirrhosis: The Best Guide and Diet Insights
Table of ContentsFast factsFatty Liver DiagnosisStages and Progression of CirrhosisHow Fatty Liver Leads to CirrhosisTreatments for Fatty LiverManaging Cirrhosis MedicallyMeal…
The Link Between Laxatives and Dementia: You Need to Know
Link between laxatives and dementia care ukWhat is the number of people living in care homes in the UK who…
The Best Guide To Powerful NLS Bioresonance Therapy for Health
Welcome to our comprehensive guide on Bioresonance Therapy, a revolutionary approach to holistic wellness. This blog post will explore the…
The 5 Interesting Hidden Links Between Stress and Constipation
Introduction Can stress and anxiety cause constipation? Chronic constipation – an often-overlooked medical conditionLet’s talk about the types and…
The Truth About Awesome Water Fasting Benefits
The concept of water fasting has emerged as a powerful antidote to reset our bodies and rejuvenate our overall well-being….
Heartburn During Pregnancy:19 Tested Ways to get relief from It
How can I relieve my heartburn while pregnant?Congratulations on the little miracle growing inside of you!It’s essential to understand that…
GERD Diet: Foods That Help with Acid Reflux (Heartburn)
Some of the questions received about the GERD Diet at the email address office@foodbodyfit.comGastroesophageal reflux disease (GERD) symptoms?Lifestyle changes and…
Is Choline the missing link for better Human Health?
Did you know that 90% of the population is at risk for a choline deficiency? Low choline intake has been…
Weight management
Weight management With the term ‘obesity’, we characterise an abnormal or excessive accumulation of body…
Nutritionist consultation
Nutritionist consultationsNutritionist consultations have a clear roadmap to recover your health, happiness and increase your energy level.What is the…
The best benefits of DMSO- The best guide that covers
Table of ContentsThe best Benefits of DMSO Unlock Your Cells’ Potential with DMSO – A Powerful Tool for Supporting Life’s…
Online Nutrition
Online Nutrition consultations provide accurate and up-to-date scientific nutrition information that can help you reach your goals. Take control of…
Osteoarthritis healing.
Osteoarthritis, full recovery without surgerySummer, 2016. Osteoarthritis healing.I woke up with severe pain in my right knee, hence I…
Best online nutritionist UK. What is a Clinical Nutritionist?
Can I see a nutritionist online?Online weight loss consultationOnline diet consultationOnline weight loss managementHow much does a nutritionist cost in…
Expert Personalised Nutrition: You Need To Know Why Everyone Is
Table of ContentsWhy Personalised Nutrition?What are the factors that can cause this difference in metabolism for two people eating the…
How Powerful Astaxanthin Empower People’s Wellness and Immunity
What is the difference between natural and synthetic astaxanthin?Astaxanthin health benefitsAstaxanthin skin benefitsFood supplement recommendationsAbsorption and bioavailabilitySafety of AstaxanthinWhat is…
DMSO a true medical miracle
THE BEST BENEFITS OF DMSO- THE BEST GUIDE THAT COVERS 31 MEDICAL CONDITIONS THAT WILL BENEFIT OF USING DMSO update…
Knee to toes. What you need to know
Management of Varicose VeinVaricose veins are twisted, dilated veins most commonly located on the lower extremities. Risk factors include chronic…
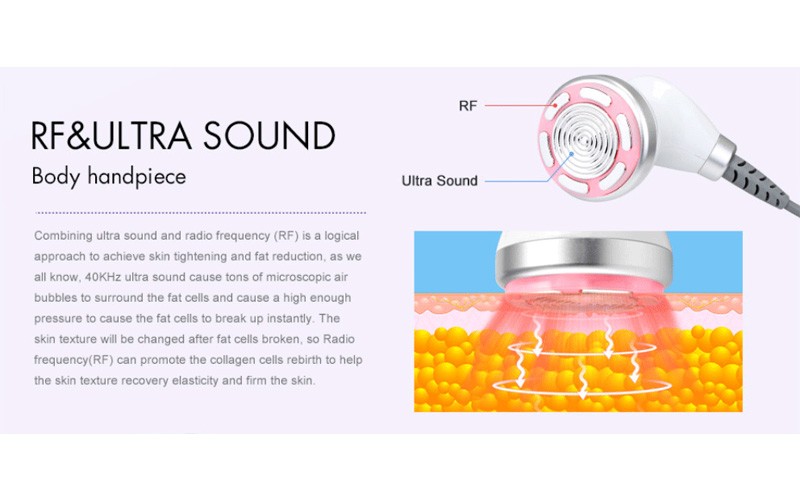
Ultrasound Fat Reduction & Weight Management
Non surgical fat reductionUltrasonic cavitation, or ultrasound cavitation, is a cosmetic procedure that’s used to break apart fat deposits in…
The sensational hidden world of CELLULAR NUTRITION
Cellular nutrition involves providing cells with the necessary materials to carry out their metabolic functions. This includes supplying them with…
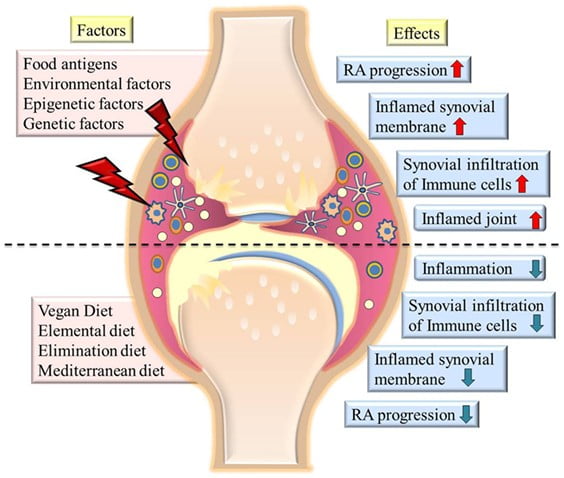
Managing Rheumatoid Arthritis with Dietary Interventions
Rheumatoid arthritis (RA) is a systemic, debilitating, chronic inflammatory autoimmune disorder affecting approximately 1% of the world population (1). The…
Osteoarthritis and nutrition
Osteoarthritis (OA) is a degenerative joint disease and a leading cause of adult disability. It can affect any joint of…
Goal setting weight management
This article provides advice on goal setting to people who are trying to make changes to their diet and lifestyle….
Eat well to heal well
Your food and fluid requirements will increase if you have a pressure ulcer or open wound. To encourage your skin…
Why do I need iron?
How do i increase iron in my diet ?How much iron do I need in my diet?Iron is important for…
13 Secrets of How to Lower Your Cholesterol Fast
Are you concerned about your cholesterol levels? Discover the secrets of lowering your cholesterol naturally through diet. Make informed decisions…
What is gastroesophageal reflux disease?
What is gastroesophageal reflux disease?GERD DIET: FOODS THAT HELP WITH ACID REFLUX (HEARTBURN)Gastroesophageal reflux disease (GORD, sometimes also known as…
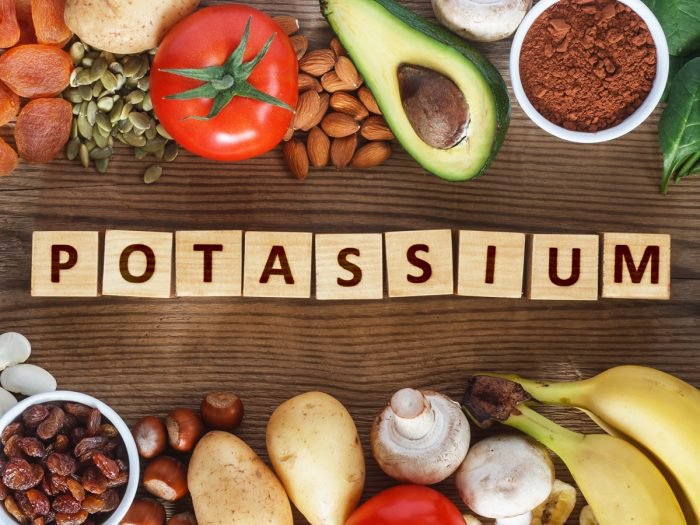
Lowering your potassium levels
Why are my potassium levels high?What is Hyperkalemia?Hyperkalemia is an excessive level of potassium in the bloodstream.Potassium has several important…
Best Advice For Lowering Your Cholesterol
High cholesterol contributes to 4.4 million annual fatalities and stands as a significant risk factor for heart disease and stroke…
Iron-Deficiency Anemia
Iron-Deficiency Anemia Anemia tends to come in two forms- pernicious anaemia and iron deficiency. If you gave pernicious anaemia , it…
Why Riboflavin is Crucial for Optimal Health and Wellness?
How it is absorbed ?Riboflavin deficiencyThe Role of Riboflavin in Homocysteine, Folic Acid and the Metabolism of Other VitaminsGroups at…
Vitamine B1 or Thiamine
Vitamine B1 or Thiamine is a water soluble vitamin, which means it is not stored in the body. A member of…
Vitamin A, retinol and beta carotene
Vitamin A Retinol and beta carotene Retinol is the naturally occurring form of vitamin A, and it is founded mainly in animal…
Causes and symptoms of Acne
Causes and symptoms of Acne Although most people associate acne with the troublesome teenage years, it can erupt at any age….
Dandelion the best natural sources of potassium
Dandelion the best natural sources of potassium Dandelion (Taraxacum officinale)I would like to introduce one of my favourite herb: dandelion. Don’t…
What is a portion? Why count calories?
What is a portion? Below are some examples of what constitutes 1 portion of each food group. A healthy balanced diet…
Signs of toxic overload
Signs of toxic overload Answer the following questions as truthfully as you can. The aim of a detox programme are to reduce…
Common illness in children and benefits of herbal medicine
Common illness in children and benefits of herbal medicine: Children’s illness, even in western medicine is widely accepted principle that the…
Benefits of Manual lymphatic drainage
Benefits of Manual lymphatic drainage(MLD) Lymphatic massage is an advanced therapy. This massage treatment is fully tailored to each individuals needs. Before…
What is herbal medicine?
Herbal medicine is used to treat the whole person. Herbal remedies create balance in the body, enabling the body’s self healing…
Women’s health
Women’s health. Plant based medicine play an important role in the lives of many women. This is because herbal remedies fulfil…
The Best VIP Bridal Weight Loss Program of 2025
Bridal Weight Loss Program 2025 by Madelena Clinical Nutritionist, Clinical Director and Women’s Health Specialist Feel Confident, Clear & Glowing on…
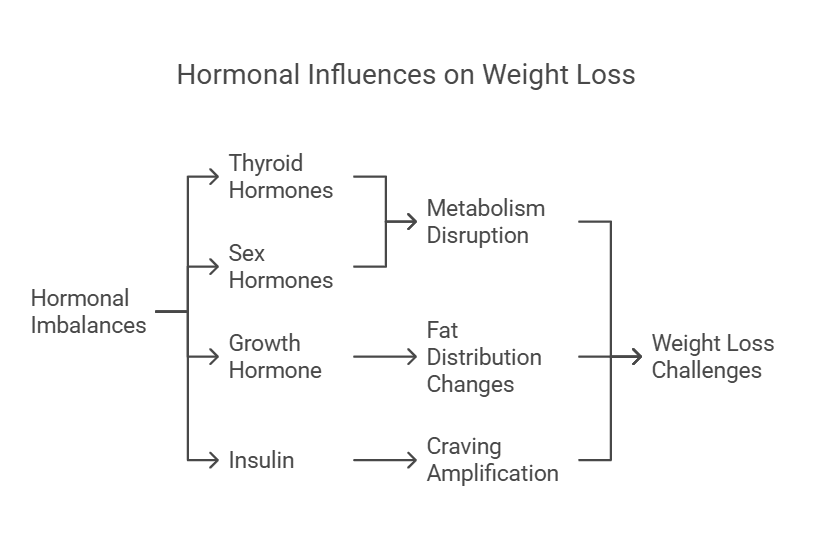
Can hormones affect weight loss? Hormonal reasons for not losing
Can hormones affect weight loss? Can hormones make it hard to lose weight?Hormonal Reasons for Not Losing WeightSigns of Hormonal…
What is Beta Glucan Mushroom Extract?
Beta Glucan Mushroom Extract Explained Beta glucans extraction from mushroomsBeta glucans mushrooms health benefitsWhich Mushrooms Contain Beta-Glucans?What is the Most Powerful…
Refund and Returns Policy
Thank you for shopping with Holistic Health Company We value your satisfaction and strive to provide high-quality supplements and services….
Why am I not losing weight on Mounjaro 10mg?
Mounjaro miracle drug?Is Mounjaro for diabetes and weight loss? Why am I not losing weight on Mounjaro 10 mg (2.5…
The Best Diet Plan After Liposuction
What to eat after liposuction?What are the best foods to eat after laser lipo?What to eat after abdominal liposuction?The Best…