Management of Varicose Vein
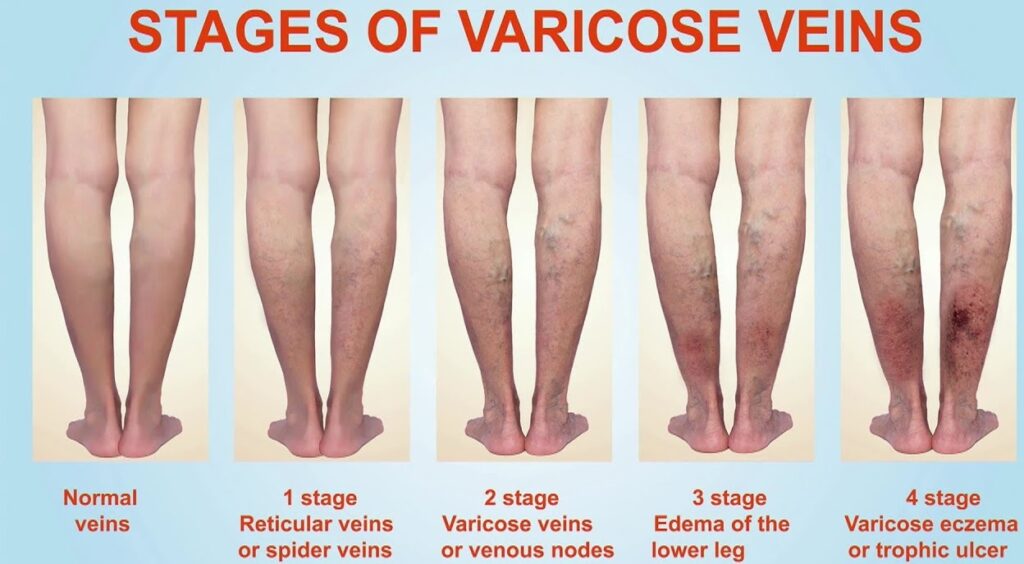
Varicose veins are twisted, dilated veins most commonly located on the lower extremities. Risk factors include chronic cough, constipation, family history of venous disease, female sex, obesity, older age, pregnancy, and prolonged standing. The exact pathophysiology is debated, but it involves a genetic predisposition, incompetent valves, weakened vascular walls, and increased intravenous pressure. A heavy, achy feeling; itching or burning; and worsening with prolonged standing are all symptoms of varicose veins. Potential complications include infection, leg ulcers, stasis changes, and thrombosis. Some conservative treatment options are avoidance of prolonged standing and straining, elevation of the affected leg, exercise, external compression, loosening of restrictive clothing, medical therapy, modification of cardiovascular risk factors, reduction of peripheral edema, and weight loss. More aggressive treatments include external laser treatment, injection sclerotherapy, endovenous interventions, and surgery.
Why legs matter
Our legs and feet do a lot for us but often they do not get the attention they deserve. Its really important that we keep an eye on our lower legs and feet. Even the smallest change to the way they look or feel can be a sign of something more serious.
The little things normal for
According to one of observational study (2019) Patients with chronic venous leg ulcers showed significantly higher BMI, hyperhomocysteinaemia, and higher levels of serum copper but significantly lower levels of vitamin B6, B9 and C, as well as a significantly lower level of zinc. Vitamin D deficiency was present in both groups, however, severe vitamin D deficiency was present only in the leg ulcer group. Mobility was significantly reduced in patients with leg ulcers.
Conclusion: Ulcer patients are often obese but suffer from qualitative malnutrition, including a lack of vitamin D, which might be explained by reduced mobility and being housebound. Hypoalbuminaemia, as a sign of protein deficiency, was observed significantly more often in patients with chronic leg ulcers, irrespective of wound area or wound duration.
This idea of a nutritional approach should be integrated into the therapeutic strategy of any wound, especially in elderly patients. In fact, age, with the associated decrease in taste and appetite, as well as problems with chewing, is a major risk factor for malnutrition. Malnutrition results not only from low calorie intake, but also from a lack of micronutrients. In other words, obesity, which is so common in our patients with leg wounds, can be accompanied by a nutritional deficit due to a diet poor in vitamins and essential amino acids. Patients who live alone, suffer from depression or have little mobility for shopping and preparing food are also at risk of malnutrition.
Interestingly, there is an overlap of risk factors for malnutrition and venous ulcers: age, obesity, social isolation, depression, poor mobility. And it is in a vicious circle, so a psychosocial approach is essential for the holistic treatment of these patients.
Nutrition is important for vein health
Chronic venous insufficiency and varicose veins appear to be related to an obesity-promoting Western lifestyle poor in dietary fiber and low in physical activity. Evidence suggests that avoidance of these risk factors may reduce the incidence of venous disorders.

High-Fiber Diets
Foods High in Rutin
Many specialists agree that the best foods for varicose veins are those high in rutin. The miraculous flavonoid has an array of benefits that has many effects on the body. One of the most essential is the ability to strengthen capillaries that are weak and most apt to develop varicose veins. As well, rutin is a vasoprotective (protects of blood vessels), anti-inflammatory, antithrombotic, (protect against blood clots) and antioxidant. Natural sources of rutin are apple, buckwheat, grapes, cherries, apricots and blackberries.
Avoidance of Overweight
Botanical Treatments
Horse chestnut seed (Aescin). The active component (aescin) appears to promote blood circulation and may strengthen the elasticity of veins. The common dosage of horse chestnut is 300 mg twice daily, containing 50 mg of Aescin in each dose.
Evidence suggests that venous insufficiency and varicose veins may be, in part, preventable through a high-fiber, low-fat diet; regular exercise; and maintenance of normal body weight. Medical, surgical, and botanical approaches are available for treatment.
Risk Factors
Family history. 90% risk of developing varicose veins if both parents have varicose veins, but less than a 20% risk if neither parent is affected.[1],[2]
Female gender. Venous insufficiency and varicosities occur up to twice as often in women as men.
Tall height. The association with height is thought to be due to the effect of gravity and pooling of blood in the lower extremities.
Advanced age.
Previous venous damage. History of leg injury, phlebitis, deep vein thrombosis, venous wall degeneration (e.g. aneurysms), arteriovenous shunts, or non-thrombotic iliac vein obstruction raises the risk for venous insufficiency.[3],[4]
Lifestyle factors. Prolonged standing, sedentary lifestyle, smoking, and pregnancy are suspected risk factors for the development of varicose veins, and obesity raises risk for venous disorders.[5] Physical inactivity is associated with risk for chronic venous insufficiency and varicose veins in some, although not all studies.[2],[6],[7]
High estrogen states and pregnancy also contribute to increased risk for developing venous insufficiency.
Klippel-Trenaunay-Weber syndrome. This rare congenital condition occurs due to an abnormal or absent deep venous system and results in a triad of extensive unilateral varicose veins, limb hypertrophy, and one or more port-wine stains.
Treatment
Initial conservative management is recommended for most patients. Bed rest, leg elevation, and compression stockings or bandages improve blood flow, reduce inflammation and edema, and compress dilated veins.
Leg elevation above the level of the heart for 30 minutes three or four times per day increases blood flow velocity, thus improving cutaneous microcirculation, and reduces edema in patients with chronic venous disease.
Exercise, such as daily walking and progressive resistance exercise up to three times per week, contributes to improvement in hemodynamic parameters and function. When combined with usual care such as compression, exercise has been shown to improve venous leg ulcer healing at 12 weeks
Compression stockings act by decreasing venous pressure and reflux. T
Several drug therapies have been used. Diuretics may be used in patients with severe edema resulting from medical conditions that exacerbate lower extremity symptoms. Oral antibiotics may be used to accelerate the healing of venous ulcers.
Venous ablation by injection sclerotherapy is useful in some patients with varicose veins for whom conservative therapies have failed. Laser therapy is the only option for treatment of telangiectasias that are too small for injection.
Several surgical options are available and have high success rates. These include venous ligation with or without stripping, endovenous catheter ablation, and valvular reconstruction.
Madelena Tapliga
MSc Clinical Nutritionist, accredited Nutritionist of UK from Association for Nutrition (AfN)
Herbal Medicine
MLD therapist
To schedule an appointment, call 07947887043 or click here to use our online form.
References
- Criqui MH, Jamosmos M, Fronek A, et al. Chronic venous disease in an ethnically diverse population: the San Diego Population Study. Am J Epidemiol. 2003;158(5):448-56. [PMID:12936900]
- Lee AJ, Evans CJ, Allan PL, et al. Lifestyle factors and the risk of varicose veins: Edinburgh Vein Study. J Clin Epidemiol. 2003;56(2):171-9. [PMID:12654412]
- Browse NL. The etiology of venous ulceration. World J Surg. 1986;10(6):938-43. [PMID:3798942]Back to Citation
- Browse NL, Burnand KG. The cause of venous ulceration. Lancet. 1982;2(8292):243-5. [PMID:6124673]
- MacKay D. Hemorrhoids and varicose veins: a review of treatment options. Altern Med Rev. 2001;6(2):126-40. [PMID:11302778
- Jawien A. The influence of environmental factors in chronic venous insufficiency. Angiology. 2003;54 Suppl 1:S19-31. [PMID:12934754]Back to Citation
- Brand FN, Dannenberg AL, Abbott RD, et al. The epidemiology of varicose veins: the Framingham Study. Am J Prev Med. 1988;4(2):96-101. [PMID:3395496]Back to Citation
[wpforms id=”0″ title=”false” description=”false”]
