Table of Contents
Do you hide your diabetes symptoms?
Diabetes Mellitus type 2 affects millions of people worldwide (537 million in 2021)
I have been asked: “Is diabetes a nutritional deficiency disease?” and “What nutrient deficiency causes diabetes?” Can a deficiency in specific nutrients lead to the development of type 2 diabetes?
This article is focused on some of the minerals and trace element deficiencies and their consequences in diabetes and insulin resistance.
There are several misconceptions surrounding nutrition and diabetes that should be addressed. Therefore, a significant number of individuals with diabetes often find themselves perplexed by contradictory nutritional guidance and viewpoints.
It’s crystal clear: Nutrition plays a crucial role in managing and preventing type 2 diabetes by impacting weight and metabolic control.
But let’s be real, when it comes to managing type 2 diabetes, figuring out nutrition can be super tricky and pretty controversial too. I’m astonished by the amount of misleading and confusing information and the surge of “health gurus” popping up like mushrooms after the rain.
Let’s review the 8 most important nutrients that may be missing in individuals with diabetes, and how they can impact the disease.
Type 2 Diabetes Nutritional Deficiency: Exploring Causes, Supplements, and Prevention Strategies
More than five million people in the UK are living with diabetes, which is an all-time high.
Diabates.UK
Our data shows that more 4.3 million people in the UK live with diabetes. Additionally, 850,000 people could be living with diabetes who are yet to be diagnosed.
These registration figures for 2021-22 are up by 148,591 from 2020-2021
The four major classes of micronutrients are macro elements, vitamins, trace elements, and organic acids. Macro elements such as chloride, calcium, and iron, along with trace elements like cobalt and zinc, play crucial roles in bodily functions, including enhancing insulin action.
Nutrition therapy is key for diabetes management and self-care education. It is widely recognized that diabetes can result from either an insufficiency in insulin secretion or from insulin resistance.
Nutritional deficiencies have been linked to the development and progression of type 2 diabetes. In particular, certain nutrients such as magnesium, zinc, vitamin D, and chromium play an essential role in maintaining sugar metabolism, blood pressure, and overall health in individuals with diabetes.
Did you know?
Global health issues affecting over a billion people are linked to deficiencies in essential minerals and trace elements such as iodine, selenium, zinc, calcium, chromium, cobalt, iron, boron, and magnesium..

A well-balanced diet and lifestyle interventions are crucial in managing type 2 diabetes, and addressing any underlying nutritional deficiencies can often provide significant improvements. Magnesium, found in whole grains, leafy greens, and nuts, is known to help improve insulin sensitivity and has been considered an essential nutrient to support healthy blood pressure. Among different forms of magnesium, magnesium citrate has been shown to aid in managing insulin resistance and blood pressure in people with diabetes.
Key Takeaways
- Nutritional deficiencies, specifically in magnesium, zinc, vitamin D, and chromium, have been shown to contribute to the development and progression of type 2 diabetes. These nutrients are crucial for regulating sugar metabolism, blood pressure, and overall health in individuals with diabetes.
- Type 2 diabetes is closely linked to nutritional deficiencies, and addressing these can improve insulin resistance and overall health.
- Magnesium citrate is essential for improving insulin sensitivity and maintaining healthy blood pressure in diabetics.
- A balanced diet and lifestyle interventions play a significant role in the successful management of type 2 diabetes and in preventing complications.
Is Diabetes A Nutritional Deficiency Disease?
Causes and Risk Factors
Minerals and trace elements are vital micronutrients found in small amounts in the body. Regional disparities in the dietary presence of selenium, zinc, copper, iron, chromium, and iodine are observed in developed and developing nations, primarily attributable to malnutrition and reliance on local food sources. These general deficiencies, and in certain instances, surpluses of crucial trace elements, can result in disturbances in glucose homeostasis and insulin resistance1.

Type 2 diabetes mellitus is strongly associated with lifestyle factors like diet, physical activity, and the use of alcohol and tobacco, along with obesity and genetic predisposition. Additionally, family history of the disease and certain ethnicities, such as African, Asian, and Hispanic, are known to have a higher prevalence of type 2 diabetes.
In the pathogenesis of type 2 DM, a relationship between glycemic control, oxidative stress, and vascular complications has long been recognized.

Diabetes mellitus (DM) is globally acknowledged as a metabolic and endocrine disorder that significantly impacts the metabolism of carbohydrates, lipids, and proteins.
The Role of Insulin
Insulin is a hormone produced by the pancreas, playing a vital role in regulating blood sugar levels. Insulin functions as a key, unlocking cells to facilitate the transfer of sugars from our bloodstream.
In those with type 2 diabetes, the body becomes resistant to insulin, or the pancreas does not produce enough insulin to maintain normal blood sugar levels. This deficiency results in high blood sugar. Poor control of blood sugar can cause multiple complications if left untreated. While type 2 diabetes is not solely caused by nutritional deficiencies, a healthy diet and lifestyle can significantly reduce the risk of developing the condition.
Diagnosis
Detecting prediabetes and making appropriate lifestyle changes can play a significant role in preventing type 2 diabetes. Early diagnosis is crucial, as effective management of type 2 diabetes can prevent or delay complications.
Adults at high risk should undergo HbA1c screening every 3 to 5 years, while those at very high risk should be screened yearly.
A diagnosis typically involves blood sugar level tests, such as fasting plasma glucose or oral glucose tolerance test.
Recent studies have conclusively shown that lifestyle changes can effectively prevent type 2 diabetes in high-risk individuals.
Research, including the Diabetic Control and Complication Trials (DCCT) and the United Kingdom Prospective Diabetes Study (UKPDS), has conclusively shown that the maintenance of blood glucose levels close to normal significantly reduce the risk of chronic complications related to diabetes.
What Nutritient Deficiencies Causes Diabetes?
Impact of Diet on Type 2 Diabetes
Unhealthy eating habits, including the consumption of refined carbohydrates, sugar-sweetened beverages, and processed meats, have been linked to an increased risk of developing diabetes. A healthy diet consisting of whole grains, fruits, vegetables, and low-glycemic foods can contribute to better blood glucose management and reduce the likelihood of complications.
Key Nutrients and Diabetes Management
Managing diabetes effectively requires focusing on key micronutrients and vitamins for blood glucose control and overall health. Some of these nutrients include:
- Magnesium: Magnesium deficiency is common among patients with Type 2 diabetes and plays a critical role in insulin sensitivity and blood pressure regulation. Magnesium citrate is often recommended as an effective form of magnesium for improving insulin resistance and managing high blood pressure.
- Vitamin D: Low levels of vitamin D have been associated with an increased risk of diabetes and insulin resistance. Supplementing with vitamin D may help improve blood glucose management and reduce the risk of complications.
- Chromium: Chromium is a trace mineral that enhances the action of insulin, facilitating glucose uptake into cells, beneficial for depression too. Chromium nicotinate and picolinate have the best absorption, compared with Chromium chloride. The highest concentrations are: found in the liver, kidneys, and spleen, while slightly lower levels are observed in heart, muscle, pancreas, lungs, bones and brain. Be kind to your liver 🙂
- B Vitamins: B vitamins, such as thiamine, niacin, and biotin, play essential roles in carbohydrate metabolism and energy production. In individuals with diabetes, B vitamins may offer protective effects against diabetic neuropathy and other complications.
It’s important to note that supplementation with these nutrients should be done under the guidance of a healthcare professional.
A balanced diet focused on whole foods is the best approach for achieving adequate levels of essential nutrients and vitamins, and preventing nutritional deficiencies related to diabetes.
Best Magnesium for insulin resistance
Magnesium and Blood Sugar Regulation
Magnesium is the fourth most abundant mineral, crucial for over 300 metabolic reactions, and essential for many cellular processes. Some of the processes in which magnesium is a cofactor include but are not limited to, protein synthesis, cellular energy production and storage, reproduction, DNA and RNA synthesis, and stabilizing mitochondrial membranes.
Magnesium is crucial for nerve function, heart health, muscle movement, blood pressure regulation, and metabolism of glucose and insulin.
Magnesium is crucial for disease prevention and overall health due to its numerous functions in the body.


Low levels of magnesium have been associated with several chronic diseases including:
migraine headaches, Alzheimer’s disease, cerebrovascular accident (stroke), hypertension, cardiovascular disease, and type 2 diabetes
mellitus.
Intracellular Mg plays a key role in regulating insulin
action, insulin-mediated-glucose-uptake and vascular
tone
Type 2 diabetes mellitus is often linked with changes in magnesium (Mg) status.
An increased incidence of magnesium (Mg) deficiencies has been documented in individuals diagnosed with type 2 diabetes mellitus (DM2), especially among patients with inadequately controlled glycemic levels, those with an extended duration of the disease, and subjects experiencing micro- and macrovascular chronic complications.
Decreased magnesium levels were also correlated with a higher incidence of arrhythmias in obese subjects with DM2, and were linked to a more accelerated deterioration of renal function.
Some key points regarding the relationship between magnesium and blood sugar regulation include:
- Magnesium is involved in the synthesis, release, and action of insulin.
- Magnesium deficiency can impair insulin sensitivity and lead to increased insulin resistance.
- Low magnesium levels may contribute to decreased glucose tolerance and higher blood sugar levels.
Magnesium Citrate and Insulin Sensitivity
Magnesium citrate is a specific form of magnesium commonly used as a dietary supplement due to its high bioavailability. It has been shown to improve insulin sensitivity and potentially help type 2 diabetes management2.
Some noteworthy benefits of magnesium citrate include:
- Magnesium citrate supplementation has been demonstrated to improve glycemic control in people with type 2 diabetes, allowing for better blood sugar regulation.
- Magnesium citrate may help mitigate insulin resistance, a key factor in the development and progression of type 2 diabetes.
- Including magnesium-citrate-rich foods or supplements in one’s diet could potentially reduce the risk of developing type 2 diabetes and its associated complications.
In conclusion, magnesium plays a crucial role in metabolic control and blood sugar regulation, making it an essential nutrient for individuals with type 2 diabetes. Ensuring adequate magnesium intake through diet or supplementation, such as with magnesium citrate, can help improve insulin sensitivity and glycemic control in patients with this chronic condition.
Diabetes Zinc Deficiency
Zinc is an essential trace element that plays a vital role in various bodily functions, including immune response, growth, and development, as well as maintaining proper insulin function. Zinc plays a crucial role in cellular signaling and processes, including cell division and apoptosis. Disruptions in zinc homeostasis are linked to diabetes and insulin resistance.
Diabetes and zinc deficiency are common issues, which have been associated with poor glycemic control and other complications related to the disease.
Diabetes, insulin and zinc have a complex correlation.
Several studies have highlighted the impact of zinc deficiency on diabetes, due to its role in insulin function and glucose metabolism. Food rich in zinc include seafood, beans, whole grains, and nuts. Individuals with diabetes must ensure adequate zinc intake through their diet or supplements.
In a cross-sectional study, findings show low zinc level is related to poor glycemic control in type 2 diabetes patients. Another study showed that a moderately high dietary zinc intake could reduce the risk of type 2 diabetes by 13%.
By focusing on a balanced diet and working closely with healthcare providers, individuals with diabetes can work towards healthier outcomes and improved disease management.
Vitamin D Diabetes Mellitus
Increasing evidence shows that vitamin D might play a role in various health issues beyond our bones, like heart disease, cancer, autoimmune diseases, and type 2 diabetes. The idea that vitamin D might play a role in managing type 2 diabetes comes from noticing that blood sugar control in people with type 2 diabetes tends to be worse in winter when a lack of vitamin D is more common3.
Vitamin D plays a crucial role in regulating the body’s absorption of calcium and phosphorus, essential for the normal development and maintenance of healthy bones and teeth.
Recent studies show that vitamin D and calcium balance might be the key player for neuromuscular function and falls, managing psoriasis, multiple sclerosis, and colorectal and prostate cancer.
It is also involved in immune system regulation and the proper functioning of insulin-producing cells in the pancreas. The connection between vitamin D and type 2 diabetes has been the subject of numerous studies, with some suggesting that a deficiency may be linked to the development of the condition.
A review of the available literature indicated the evidence regarding the link between vitamin D deficiency and type 2 diabetes. The study found that individuals with higher intakes of dietary calcium and vitamin D had a significantly reduced risk of developing type 2 diabetes. However, the authors caution that more research is needed to confirm these findings.
In another study, vitamin D supplementation was provided to participants at high risk for type 2 diabetes. The results showed that a daily dosage of 4000 IU of vitamin D3 did not significantly lower the risk of diabetes compared to a placebo.

Individuals with type 2 diabetes or at high risk for developing the disease are often encouraged to maintain a balanced diet that includes foods rich in vitamin D. Some of these foods include
- Fatty fish (such as salmon, trout, tuna, and mackerel)
- Beef liver, cheese, and egg yolks have small amounts of vitamin D, primarily in the form of vitamin D3 and its metabolite 25(OH)D3.
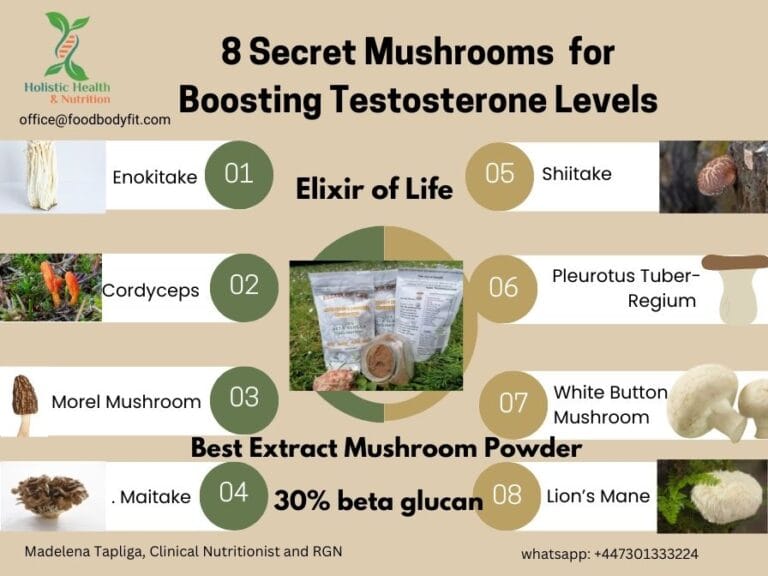
- Mushrooms are another source of Vitamin D2. Some mushrooms on the market undergo UV light treatment to enhance their vitamin D2 content. However, my recommendation is to buy Best Mushroom Supplement for Diabetes Elixir of Life Best Mushroom Supplement for Health. Have you been wondering which mushroom is best for diabetes?
- Fortified foods (such as milk and orange juice)
It is important to remember that the relationship between vitamin D and type 2 diabetes is still being studied, and results could vary based on population, study design, or dosage used in interventions. However, maintaining adequate vitamin D levels through diet and supplementation is always important for overall health.
Vitamin E and Diabetes
Vitamin E, this essential fat-soluble vitamin functions primarily as an antioxidant, it helps protect the body’s cells against damage by free radicals, which are associated with the development of chronic diseases.
Free radicals can contribute to various diseases like heart disease and cancer, not to mention they play a part in the normal aging of our cells.
Low levels of vitamin E have been linked to a higher prevalence of diabetes, and existing research indicates that individuals with diabetes may exhibit reduced levels of antioxidants.
Vitamin E has been studied for its role in improving insulin resistance and glycemic control.
Some of the key functions of vitamin E regarding diabetes management include:
- Vitamin E supplementation can significantly decrease plasma glucose and hemoglobin A1c (HbA1c) levels
- Preventing oxidative damage: The oxidative damage brought on by diabetes is thought to be reduced when vitamin E is present, as it acts as a chain-breaking inhibitor of lipid peroxidation.
- Enhancing insulin sensitivity: Studies have shown that vitamin E supplementation has beneficial effects on insulin resistance and possesses the potential to improve glycemic control in individuals with type 2 diabetes.
- Decrease the risk of diabetic complications: Vitamin E helps control oxidative stress and, manage diabetes complications like neuropathy and retinopathy.

Moreover, addressing a possible vitamin E deficiency is important for those with diabetes. Foods rich in vitamin E include:
- Nuts and seeds are good sources of vitamin E. (e.g., almonds, sunflower seeds, and hazelnuts)
- Vegetable oils (e.g., sunflower, safflower, and wheat germ oil). Regarding vegetable oils such as sunflower, please go to cold press sunflower
- Includes a variety of protein foods such as lean meats; poultry; eggs; seafood; beans, peas, lentils; and non-GMO soy products
- Avocado, Broccoli
- Green leafy vegetables (e.g., spinach, kale, and Swiss chard)
If you’ve got type 2 diabetes, getting enough Vitamin E is a game changer. It not only boosts your overall health but also helps you manage your blood sugar levels better.
Calcium and Diabetes

Calcium homeostasis plays significant roles in insulin resistance and secretion, with implications for diabetes management. Research suggests associations between low vitamin D status, calcium intake, and the prevalence of type 2 diabetes mellitus (T2DM) or metabolic syndrome. Serum calcium levels may fluctuate in diabetic patients, potentially influencing glycemic control. Cohort studies indicate a correlation between elevated serum calcium levels and an increased risk of diabetes, independent of various factors.
- Observational studies suggest a consistent association between low vitamin D status, calcium or dairy intake, and prevalent type 2 diabetes or metabolic syndrome.
- Meta-analyses indicate inverse associations between incident type 2 diabetes or metabolic syndrome and combined vitamin D and calcium intake or dairy intake.
- 💊 Trials with vitamin D and/or calcium supplementation suggest potential benefits in preventing type 2 diabetes, particularly in high-risk populations like those with glucose intolerance.
- Optimizing vitamin D and calcium intake might help in improving glucose metabolism and glycemia.
- 🔍 Understanding the mechanisms linking vitamin D and calcium to type 2 diabetes involves exploring their roles in pancreatic β-cell function, insulin sensitivity, and systemic inflammation.
- 🥛 Dairy intake is inversely associated with fasting plasma glucose, indicating a potential benefit in managing metabolic syndrome.
- Calcium supplementation, especially as part of dairy products, shows conflicting results in trials regarding its effect on glycemia or insulin resistance.
- 💡 Dietary calcium regulation may impact adiposity and body weight.
It is interesting to note that in individuals without type 2 diabetes, the daily mean intake levels of calcium and magnesium are found to be around 960 mg and 300 mg, respectively. However, for people with diabetes, these numbers drop to 890.3 mg of calcium and 278.9 mg of magnesium per day.
Understanding and maintaining calcium balance may have implications for diabetes prevention and management.
Personalised nutrition is crucial when it comes to managing diabetes and achieving weight loss goals. This approach takes into consideration an individual’s unique nutritional needs, health goals, lifestyle habits, and food preferences. With diabetes being a complex disease, having a personalized nutrition plan can help individuals better manage their blood sugar levels and prevent potential complications.
Chromium and diabetes
Did you know in the late 50s, Schwarz and Mert first discovered that chromium plays a role in controlling blood sugar?
Chromium is a vital nutrient that plays a critical role in glucose metabolism, by enhancing the binding of insulin to INSR (insulin receptor), insulin, and blood lipids. Inadequate dietary consumption of chromium is linked to elevated risk factors for diabetes and cardiovascular diseases.
Consuming large amounts of sugar, engaging in exhaustive physical exercise, and phases like pregnancy and lactation can lead to increased Chromium excretion in humans.
Signs of Chromium deficiency: include elevated blood glucose, insulin, cholesterol and, triglycerides, and decreased high-density lipoproteins (HDL) in humans consuming normal diets.
Chromium deficiency is often linked to the onset and progression of diabetes and its complications [1].
Serum levels of Chromium are lower in diabetic and obese patients.
Have you been tested for Chromium level?
Steroid-induced diabetes is reported in 2 to 46% of patients undergoing kidney transplantation

More severe signs of Chromium deficiency (including nerve and brain disorders) that are reversed by supplemental Cr was reported for patients on total parenteral nutrition (TPN) Chromium is now routinely added to TPN solutions.
- Chromium alleviates glucose intolerance.
- Chromium alleviates Type 2 DM and gestational diabetes.
- Chromium increases insulin receptor phosphorylation.
- Chromium is a safe nutrient supplement
- Improved lipid metabolism, subsequently reducing the risk of cardiovascular complications, which are often associated with diabetes4
Taking Cr picolinate supplements has been shown to significantly improve blood glucose, insulin levels, cholesterol, and hemoglobin A1C in individuals with Type 2 diabetes, with the benefits increasing alongside the dose.
Incorporating chromium in the diet can be achieved through various food sources such as whole grains, broccoli, green beans, nuts, and lean meats. However, due to the lower bioavailability of chromium from food sources, some individuals might benefit from supplemental sources such as chromium picolinate or chromium polynicotinate to assist in managing their diabetes5.
It is essential to note that chromium’s efficacy and optimal dosage for addressing type 2 diabetes may vary among individuals.
Before starting chromium supplementation consult with a healthcare professional.
In conclusion, chromium plays an essential role in managing type 2 diabetes due to its beneficial effects on insulin sensitivity and glucose regulation. Adequate chromium intake through diet or supplements can help alleviate the symptoms of diabetes and reduce the risk of complications.
Low Iodine and Diabetes
Thyroid function is essential for regulating energy metabolism, and abnormal thyroid function may substantially affect blood glucose control in diabetes.
Iodine is a crucial micronutrient that is vital in producing thyroid hormones.
People with diabetes have a higher chance of getting thyroid problems.
It has been observed that deficiencies in minerals and trace elements, including iodine, can have a significant impact on the development of metabolic disorders, including type 2 diabetes, gestational diabetes, and high blood pressure
During pregnancy and early infancy, iodine deficiency can lead to irreversible consequences.
Gestational diabetes iodine
Gestational diabetes mellitus (GDM) is a condition that is characterized by glucose intolerance with onset during the pregnancy and which might attenuate after delivery. However, GDM increases the risk of diabetes mellitus type 2.

Recent studies have shown that iodine is linked to glucose metabolism, glucose intolerance, impaired fasting glucose, prediabetes, diabetes mellitus, or gestational diabetes.
Furthermore, reduced thyroid hormone levels during pregnancy have been proposed as a potential risk factor for gestational diabetes mellitus (GDM). Therefore, the French National Authority for Health (HAS) and the World Health Organization (WHO) recommend iodine supplementation during pregnancy.
Clinicians and healthcare professionals should keep in mind that managing iodine deficiency is complex and needs careful planning, even before pregnancy.
It is essential to maintain an adequate intake of iodine through food sources like seaweed, seafood, and dairy products to avoid deficiency Individuals at risk of iodine deficiency, such as pregnant women and people living in regions with low iodine levels in the soil, should pay special attention to their iodine intake.
Ensuring a sufficient iodine intake through a balanced diet and supplementation if necessary is essential to prevent deficiency and its related complications.
Given the plausible interconnection between iodine, thyroid function, and glucose homeostasis, coupled with the global epidemiological status of iodine deficiency and Type 2 Diabetes Mellitus prevalence, further research is important.
Diabetes and iron overload
Iron is essential for various bodily functions, including physical growth, neurological development, and hormone synthesis. Iron absorption primarily occurs in the duodenum and jejunum, facilitated by ferroportin, a transmembrane protein. The body’s iron stores are regulated through a balance of dietary intake, absorption, recycling from old red blood cells, and storage within macrophages.
- Iron plays a crucial role in the pathophysiology of various diseases due to its ability to generate reactive oxygen species.
- Increased iron levels have been associated with the induction and complications of diabetes, including diabetic nephropathy and cardiovascular disease.
- Genetic iron overload syndromes like hereditary hemochromatosis are linked to an increased risk of diabetes, suggesting a role for iron in abnormal glucose metabolism.
- Transfusional iron overload, dietary iron intake (particularly from red meat), and other conditions like hepatitis C virus infection and porphyria cutanea tarda can contribute to diabetes.
- Mechanisms through which iron contributes to diabetes include insulin deficiency, insulin resistance, and hepatic dysfunction.
- There’s evidence suggesting a relationship between iron and diabetic complications such as microangiopathy and atherosclerosis.
- Iron chelation therapy presents a potential avenue for interrupting iron-induced oxidative stress and preventing diabetes-related complications.

Dietary strategies may indirectly help manage iron levels and potentially reduce the risk of diabetes:
- Limit Red Meat Consumption: Red meat is a significant source of heme iron, which is more readily absorbed by the body compared to non-heme iron found in plant-based sources. Reducing the intake of red meat, particularly processed varieties, may help lower overall iron intake.
- Increase Consumption of Plant-Based Foods: Plant-based foods contain non-heme iron, which is less readily absorbed by the body. Including more fruits, vegetables, legumes, and whole grains in the diet can provide iron without significantly increasing iron stores.
- Pair Iron-Rich Foods with Vitamin C: Consuming foods rich in vitamin C alongside iron-rich foods can enhance the absorption of non-heme iron. Examples include pairing iron-fortified cereals with citrus fruits or adding bell peppers to bean salads.
- Monitor Iron Levels: For individuals at risk of iron overload or with a family history of hereditary hemochromatosis, regular monitoring of iron levels through blood tests is essential. This allows for early detection and intervention if iron levels become elevated.
- Consider Cooking Methods: Cooking in iron pots or pans can increase the iron content of food, particularly acidic dishes. Opting for alternative cookware materials like stainless steel or non-stick coatings may help moderate iron intake.
- Maintain a Balanced Diet and Healthy Lifestyle: Overall, focusing on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, combined with regular physical activity, can help maintain optimal health and potentially reduce the risk of diabetes.
Iron deficiency anemia
Association between type 2 diabetes mellitus and iron deficiency anemia: Several studies have highlighted associations between T2DM and alterations in iron parameters. For instance, T2DM patients, particularly women, have been observed to have lower ferritin levels compared to controls. Additionally, T2DM patients with anemia exhibit decreased levels of red blood cells (RBC) and hematocrit (HCT) compared to those without anemia.
Vitamin K and diabetes management
Vitamin K plays a crucial role in managing type 2 diabetes mellitus. It has been found that this fat-soluble vitamin may positively affect glycemic regulation and help improve insulin sensitivity. Studies indicate that increasing vitamin K intake can lower the risk of developing diabetes mellitus in the long run.

There are two primary forms of vitamin K, namely vitamin K1 (phylloquinone) and vitamin K2 (menaquinone). While vitamin K1 is predominantly available in green leafy vegetables, vitamin K2 can be found in fermented foods, animal products, and certain supplements. Incorporating these foods into the diet can provide the necessary amount of this vital nutrient.
- Vitamin K, including phylloquinone (VK1) and menaquinone (VK2), has roles beyond coagulation control, affecting various aspects of human health.
- Studies highlight the significance of vitamin K in regulating insulin resistance, glycemic state, and glucose metabolism.
- Increased dietary intake of vitamin K is associated with lower plasma concentrations of markers related to diabetes and a reduced risk of acquiring diabetes mellitus.
- Retrospective analysis shows a negative correlation between vitamin K consumption and the occurrence of type 2 diabetes mellitus over a decade.
- While menaquinones may play a role in reducing diabetes risk, evidence supporting phylloquinone’s effect is lacking.
It has been found that vitamin K enhances the function of proteins responsible for insulin secretion and utilization in the body.
Individuals with type 2 diabetes need to consume a balanced diet rich in both vitamin K1 and K2, along with vitamin K supplementation.
What food can diabetics eat freely?
Nutrition Therapy for Diabetes
A healthy diet is crucial in managing and preventing type 2 diabetes. One such diet is the Mediterranean diet, nutrient-dense food. high in whole grains, fruits, vegetables, and healthy fats such as cold pressed olive oil, avocado, nuts. It is well-known for its benefits in improving glycemic control and promoting weight loss6.
Consuming foods with a low glycemic index, like whole grains, fruits, legumes, animal proteins is recommended for individuals with DM2, while limiting refined carbohydrates.
Very-low-calorie diets provide ≤800 calories daily and produce substantial weight loss and rapid improvements in glycemia and lipemia in individuals with type 2 diabetes.
Consuming 1.0-1.5 g/kg/day of protein has shown improvements in glycemic control and muscle mass in older adults.
In addition to incorporating the Mediterranean diet, it is essential to focus on specific nutrients that could help manage diabetes.
The management of type 2 diabetes involves a combination of medications, insulin therapy (when necessary), and lifestyle modifications, including a nutritionally balanced diet and regular physical activity. Each treatment plan should be tailored to the patient’s unique needs and preferences, ensuring effective blood sugar control and a higher quality of life.
It is highly recommended for individuals with diabetes to closely monitor their nutrition therapy to maintain appropriate macronutrient and micronutrient balances. In doing so, they can effectively manage their condition and experience a better quality of life.
Physical Activity and Weight Management
A key component of managing type 2 diabetes is adopting a lifestyle that includes regular physical activity. Engaging in at least 150 minutes per week of moderate-intensity exercise, like brisk walking or cycling have been shown to improve blood sugar control and overall cardiovascular health. Physical activity also plays an essential role in weight management, as maintaining a healthy weight is crucial in preventing complications related to diabetes.
Complications of Type 2 Diabetes
Neuropathy and Heart Disease
Type 2 diabetes can lead to a variety of complications, including neuropathy and heart disease. Neuropathy, or nerve damage, can cause tingling, numbness, and pain in various parts of the body, particularly in the extremities. It is a result of high blood sugar levels over an extended period, which can damage the nerves. According to Diabetes UK, people with type 2 diabetes are at a higher risk of developing cardiovascular issues, such as heart disease and stroke.
Heart disease is a significant concern for individuals with type 2 diabetes. The BMJ article states that the risk of developing heart disease is two-fold higher in people with type 2 diabetes compared to those without the condition. It is primarily due to atherosclerotic cardiovascular disease, which can lead to complications such as heart attack, stroke, and peripheral arterial disease.
Diabetes and Blood Pressure
High blood pressure, or hypertension, is another common complication of type 2 diabetes. It is closely related to other complications such as heart disease and neuropathy. The CKS-NICE states that people with type 2 diabetes have a two-fold increased risk of developing high blood pressure.
The connection between type 2 diabetes and high blood pressure can be attributed to a few factors, such as insulin resistance, inflammation, and kidney damage caused by elevated blood glucose levels. Proper management of blood pressure is essential in people with type 2 diabetes to minimize the risk of serious complications.
For better management of blood pressure and diabetes, it is important to follow a balanced diet rich in magnesium, which plays a vital role in regulating blood pressure. Magnesium citrate supplements can help people with insulin resistance and diabetes.
Frequently Asked Questions
What type of magnesium supplementation is most beneficial for individuals with type 2 diabetes?
There are various forms of magnesium supplements available, but research suggests that magnesium citrate is one of the most easily absorbed forms for individuals with type 2 diabetes. Magnesium glycinate and magnesium chloride are other well-absorbed forms that may be beneficial for diabetic patients
What daily amount of magnesium is recommended for patients managing type 2 diabetes?
The recommended daily amount of magnesium for adults varies depending on age and gender. For men, the recommended daily allowance (RDA) is 400-420 mg, while for women, it is 310-320 mg. However, it is important to consult with a healthcare professional before starting any supplement regimen, as individual needs may vary.
Are there any nutritional deficiencies commonly associated with type 2 diabetes?
Yes, some nutritional deficiencies are more prevalent in individuals with type 2 diabetes. These include deficiencies in vitamin B12, especially among those taking metformin; as well as magnesium, vitamin D, iodine and other micronutrients. People with diabetes must maintain a well-balanced diet that meets their nutritional needs.
Conclusion
Diabetes mellitus can affect the levels of trace elements in the body, potentially impacting the nutritional status of individuals. While certain micronutrients play roles in the development and advancement of diabetes, others may be influenced by changes in carbohydrate tolerance and insulin resistance.
Healthcare professionals such as doctors, dietitians, and certified diabetes educators can provide valuable guidance in making suitable lifestyle choices.
Considering the individual needs of each patient, healthcare professionals and online resources can provide tailored advice for effectively managing type 2 diabetes throughout one’s life.
- Nutrients 2020, 12(6), 1864; https://doi.org/10.3390/nu12061864 ↩︎
- Afitska K, Clavel J, Kisters K, Vormann J, Werner T. Magnes Res 2021; 34(3): 130-139. doi: 10.1684/ mrh.2021.0489 ↩︎
- Eur J Clin Nutr. 2011 September ; 65(9): 1005–1015. doi:10.1038/ejcn.2011.118.
NIH ↩︎ - Rebecca B. Costello, Johanna T. Dwyer, Regan L. Bailey, Chromium supplements for glycemic control in type 2 diabetes: limited evidence of effectiveness, Nutrition Reviews, Volume 74, Issue 7, July 2016, Pages 455–468, https://doi.org/10.1093/nutrit/nuw011 ↩︎
- Forouhi N G, Misra A, Mohan V, Taylor R, Yancy W. Dietary and nutritional approaches for prevention and management of type 2 diabetes BMJ 2018; 361 :k2234 doi:10.1136/bmj.k2234 ↩︎
- BMJ 2018;361:k2234 doi: 10.1136/bmj.k2234 (Published 13 June 2018) ↩︎


[…] compound also appears to improve insulin sensitivity. This helps regulate blood sugar and may prevent excess fat accumulation. Nuciferine activates brown fat tissue, which burns calories […]