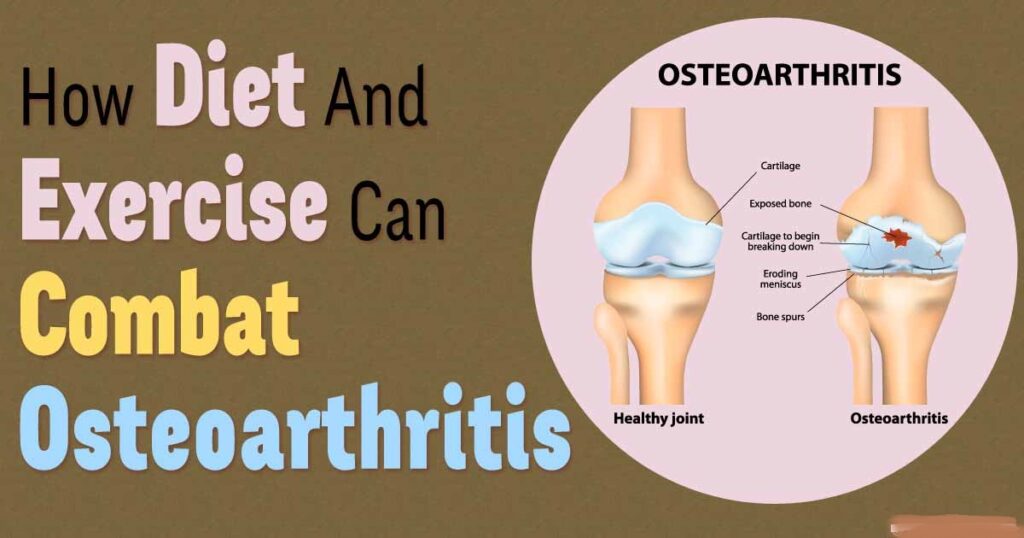
Osteoarthritis (OA) is a degenerative joint disease and a leading cause of adult disability. It can affect any joint of the body but most commonly involves the knees, hips, neck, low back, and hands.
It is estimated that degenerative joint disease disorders such as osteoarthritis will impact at least 130 million individuals throughout the globe by the year 2050. Advanced age, obesity, genetics, gender, bone density, trauma, and a poor level of physical activity can lead to the onset and progression of osteoarthritis
Current pharmacologic treatments such as analgesics and non-steroidal anti-inflammatory drugs may improve the pain and offer some relief but they do not affect the progression of the disease. It may also not adequately slow the breakdown of cartilage. The chronic intake of these drugs may result in severe adverse events.
Areas of the gastrointestinal tract that may be damaged by NSAIDs
- Oesophagus: oesophagitis, ulceration, stricture
- Stomach: ulcers, erosions
- Duodenum: ulcers, erosions
- Small intestine: ulcers, erosions, protein loss, strictures
- Colon: non-specific colitis, exacerbation of ulcerative colitis and Crohn’s disease
Over 22 million prescriptions are written every year in the UK, and over 70 million in the US.
OA is characterised by progressive degeneration of articular cartilage with resultant joint space narrowing, cyst, and osteophyte formations. In the spine, OA is additionally characterised by disk dehydration, decreased disc space. height and dysfunction, as well as facet joint hypertrophy and narrowing of the neuroforamen. OA in the knee may involve the articular cartilage of the patellofemoral, proximal tibia fibula, and tibia femur joints. OA of the knee commonly involves degenerations and tearing of meniscal cartilage on the medial or lateral meniscus, which increases risk of degeneration of the articular cartilage.
OA progresses when tissue regeneration cannot keep pace with the rate of cartilage loss. Joint damage may occur when the biomaterial properties of the articular cartilage are inadequate or load on the joint is excessive.
Questions about the role of diet in the prevention and treatment of their joint disorder may be among the most frequent posed by patients with osteoarthritis (OA). Interestingly, while there are thousands of lay publications recommending various arthritis diets, physicians have little
information to over based on scientific studies. Arguably in no other aspect of rheumatology is public and medical interest so discrepant.
Beyond physical function, OA also negatively impact mental health. Increasing evidence indicate that: patients with knee or hip OA have greater risk of depression; OA is associated with greater Odds of suicidal ideation; and OA patients show memory loss that was partially mediated by sleep and mood impairments (reviewed in [10]). Several studies evaluated the impact of OA on hard outcomes, such as cardiovascular morbidity and mortality.
Classical risk factors: OA was in the past consider an effect of aging. Today we know that pathogenesis is multifactorial including constitutive features of the joint, non-modifiable and modifiable risk factors. OA could also be a consequence of other diseases that could affect joints directly:
- Genetic factor
- Gender. OA is more common in female, especially in elderly subjects. Post-menopausal rise of OA in women and the detection of oes-trogen receptors (ERs) in joints highlight the attention on a possible roleof hormones in the pathogenesis of OA.
- Age. Prevalence of OA increases with age with a peak incidence between 55 and 64 years. During aging pro-inflammatory cytokines are increased, also due to an increase in fatmass, which can itself induce the production of adipokines and cytokines. Finally, enhancement in oxidative stress, associated with increased levels of free fatty acids (FAs) and hyperglycaemia, can promote the destruction of the tissue matrix inducing an alteration of mechanical charge and consequent damage of cartilage
- Metabolic syndrome: Epidemiological studies highlight the link between metabolic syndrome (MetS, combination of obesity, hypertension, hyperglycaemia, insulin resistance and dyslipidaemia) and OA.

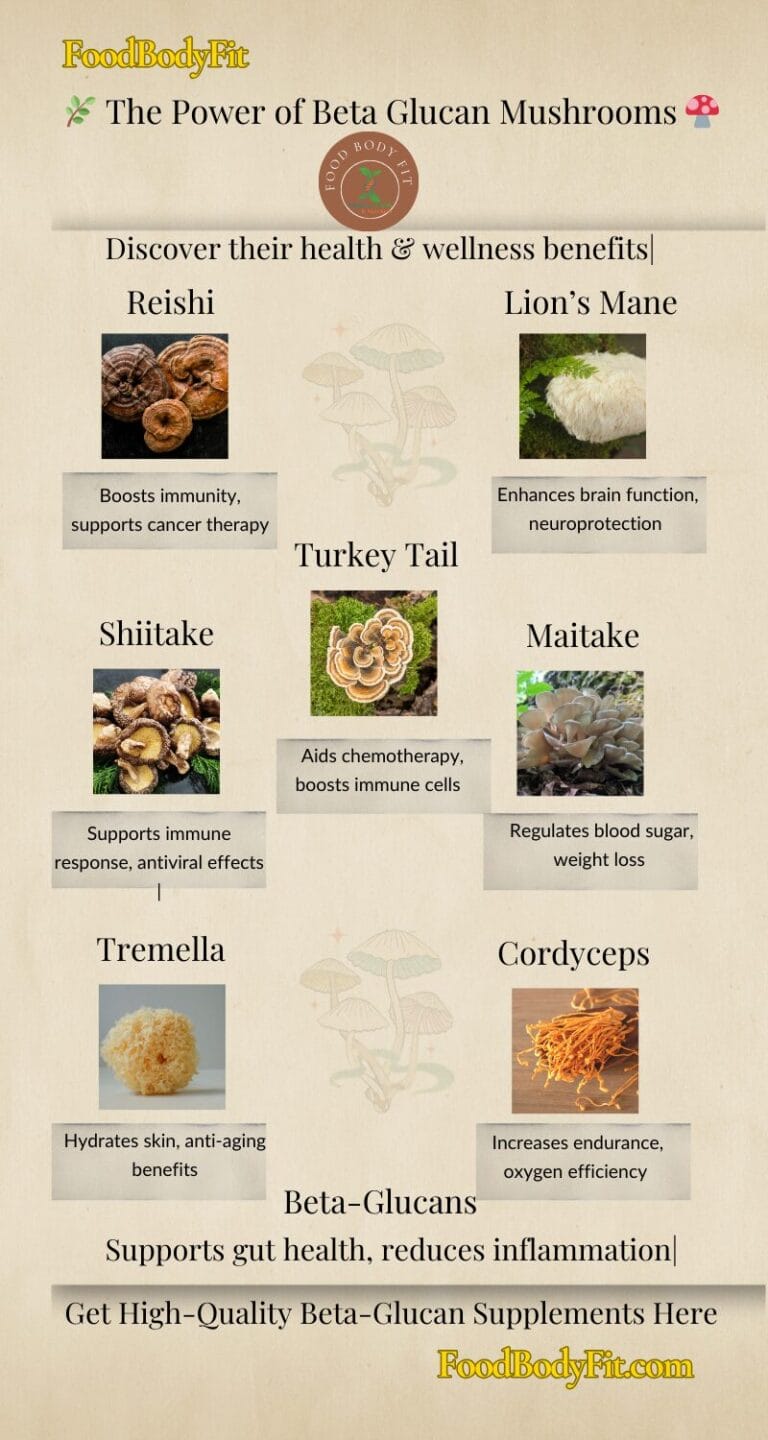
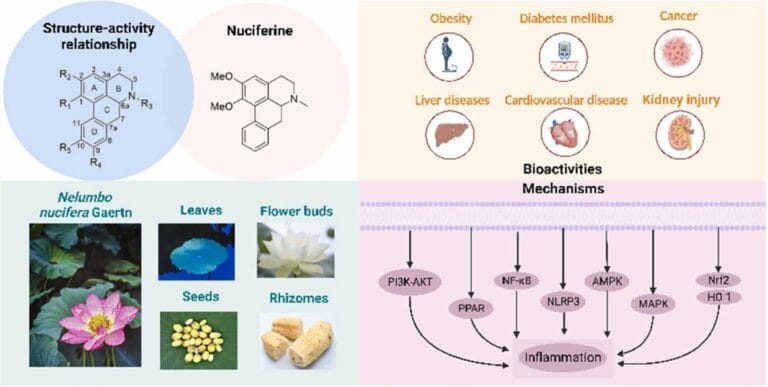
The influence of nutrients and diet on the metabolism of cartilage and OA could represent a long-term coadjuvant alternative in the management of patients with OA. Effects of diet modifications on lipid and cholesterol profiles, adequate vitamin levels and weight reduction in obese patients could influence the course of the disease
Exercises
Physical exercise and weight loss are strongly recommended (also from both European League Against Rheumatism and American College of Rheumatology guidelines) as cardinal intervention for OA prevention and treatment [
The exercise must be personalized according to the patient’s preferences and abilities, The training programs can be individual, in groups, at home or in the gym. Exercises in water or on the ground have the same value and should be preferred according the physical characteristics and preferences of the patient. A mixed approach (aerobic and strengthening) is recommended with the aim of reducing pain, improving proprioception and joint function.
Abnormal overload, both occupational or in case of extreme sport activity, could be an additional risk factor for OA. Abnormal load is not only due to overweight but also joint instability, immobilization, or trauma. Population studies highlight the role of heavy physical work as a risk factor for knee and hip OA especially for heaviest manual work (knee OR 18.3 (CI95% 4.2, 79.4), hip OR 6.7 (CI95% 2.3, 19.5))
Madelena Tapliga
MSc Clinical Nutritionist, accredited Nutritionist of UK from Association for Nutrition (AfN)
Herbal medicine
MLD therapist
References:
Bortoluzzi, Alessandra; Furini, Federica; Scirè, Carlo A (2018) Osteoarthritis and its management – Epidemiology, nutritional aspects and environmental factors. Autoimmunity Reviews, 1568-9972, . 17 (11), pp: 1097-110
Messina, O.D., Vidal Wilman, M. & Vidal Neira, L.F. Nutrition, osteoarthritis and cartilage metabolism. Aging Clin Exp Res 31, 807–813 (2019). https://doi.org/10.1007/s40520-019-01191-w
Russell RI. Non-steroidal anti-inflammatory drugs and gastrointestinal damage—problems and solutionsPostgraduate Medical Journal 2001;77:82-88.
MCALINDON T, FELSON DTNutrition: risk factors for osteoarthritisAnnals of the Rheumatic Diseases 1997;56:397-400.

Madelena has been my nutritionist since February, and I feel extremely grateful to have met her. She is a kind, welcoming and has vast knowledge about her work.
For many years I have suffered with medical issues. one of my biggest challenges I was having was with my feet and not being able to walk properly as I was always in constant pain.
Doctors where only able to prescribe an assortment of medication which only masked the pain and led to more issues.
From meeting Madelena, she was able to regularise my eating habits, advise me on what and when to eat and certain supplements and vitamins to take.
At first it was very difficult to stop eating the foods I’ve enjoyed for most of my life, but once again, she was understanding of this and worked with me to cut them down and help me overcome this.
Within a month I could feel the difference this was having on me. Movement was becoming more easier; my weight gain was reduced, and my overall well-being was improved. Although, I still take medication at present, it is dramatically decreased making the associated issues I was experiencing from the medication cease.
I am so grateful to Madeleina as she has given me back hope.
If you are thinking about using her services, I totally recommend her. Mark