Table of Contents
Reduce the stress levels in your life through relaxation techniques like meditation, deep breathing, and exercise. You’ll look and feel way better for it.” – Suzanne Somers
Does stress make you constipated?
The 5 Interesting Hidden Links Between Stress and Constipation
Different people generally have different bowel habits.
The mechanisms that control gastrointestinal function are vast and complex.
In the short term, stress causes the delicate balance of hormones and chemicals in the body to be thrown out of line. One of the most important chemical reactions taking place at a time of stress is the release of cortisol, known as the stress hormone.
Although we need cortisol to live, when it is produced in excess quantities or over a sustained time, it begins to have a detrimental effect on the body.
It interferes with the digestion of food, sometimes halting it altogether.
Stress and constipation are two common health concerns that can be more interconnected than many people realize. The impact of stress on the digestive system, particularly the occurrence of constipation, is a topic of growing interest in the medical and wellness communities. Understanding the hidden links between these two issues is important for managing overall health and well-being.
This blog post aims to shed light on the underestimated nature of chronic constipation in adults and provides potential solutions for better care.
Introduction
Let’s start with some statistics.
The total estimated annual expenditure by NHS England on constipation in the year 2018-2019 amounted to £168 million. This comprised £87 million spent directly on prescription costs and an additional £81 million in expenses related to the treatment of the 76,929 individuals (averaging 211 per day) admitted to the hospital with a final diagnosis of constipation.
Did you know that constipation affects one in three children? Unfortunately, children under the age of 15 make up about 18% of hospital admissions related to constipation. However, let’s keep in mind that this article focuses on a different aspect and won’t cover constipation in children.
Can stress and anxiety cause constipation?

Stress and constipation are closely connected, with stress often acting as a trigger for constipation. When we experience stress, our body releases stress hormones that can affect the functioning of our digestive system.
Psychological stress is known to cause bowel dysfunction.
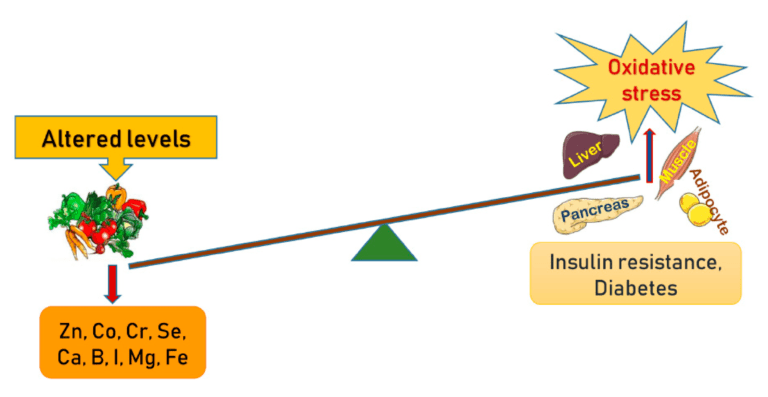
Stress can lead to changes in gut motility, slowing down the movement of stool through the intestines and causing constipation. Stress can also impact the composition of our gut microbiota, which can further contribute to constipation.
Psychological stress, such as anxiety and depression, can also play a role in the development of constipation, as they can interfere with normal bowel habits.
Understanding the relationship between stress and constipation is crucial for developing effective coping mechanisms and medical approaches to address this issue.
Chronic constipation – an often-overlooked medical condition

Chronic constipation is one of the most common gastrointestinal disorders.
Constipation is a prevalent gastrointestinal motility disorder, characterized by infrequent bowel movements (less than three times per week) and difficulty passing stool. While stress is known to have various effects on the body, its relationship with constipation is also significant.
Stress can act as a trigger for constipation, disrupting normal bowel function and causing symptoms such as hard stools and straining. Additionally, stress-induced changes in bowel habits, such as irregularity or changes in stool consistency, can contribute to constipation
Let’s talk about the types and causes of constipation! 😊
Constipation can be divided into two main types:
- Functional constipation, also known as idiopathic constipation, is constipation without any underlying non-bowel causes. The diagnostic criteria for functional constipation are provided at Rome IV Criteria.
- Neurogenic constipation occurs when there is an interference in nervous control, leading to improper bowel function. This can happen in individuals with conditions such as spina bifida, Parkinson’s disease, or those who have had a stroke.
- Constipation is a prevalent issue among patients with spinal cord injuries, with approximately one-third of individuals experiencing chronic abdominal pain a decade or more post-injury.
- The concept of neurogenic bowel dysfunction (NBD) has been introduced, comprising symptoms such as constipation, fecal incontinence, and abdominal pain.
Constipation can also be a feature of non-neurogenic diseases such as endometriosis, diabetes or underactive thyroid, or be a side-effect of medications such as opioids.
The complex connection between the brain and the gut often underpins the correlation between stress and constipation. Here are five interesting hidden links between these two seemingly disparate factors:
Emerging evidence from several studies published in The Korean Journal of Gastroenterology (Published online: August 25, 2022) points to a fascinating connection between depression and functional constipation.

1. The Gut-Brain Axis
The gut and brain communicate via the gut-brain axis, a complex network of neural, endocrine, and immune pathways.
Previous studies show the connection between mood and gastrointestinal disorders is different from other chronic illnesses due to the important role between the central nervous system and the gastrointestinal tract, also known as the brain-gut axis.
Studies on neuronal stress pathways have found that the corticotropin-releasing factor (CRF) in the brain plays a crucial role in connecting emotional distress with changes in upper and lower gastrointestinal (GI) motor function. In conditions like IBS, functional dyspepsia, and CC or diarrhea, the autonomic nervous system’s dysfunction, which directly affects CRF, may contribute to altering bowel habits and gastric emptying.
2. High Cortisol and Constipation
Does cortisol cause constipation?
Yes. It does. Stress hormone not only affect the nervous system but also play a role in digestive processes. Maintaining hormonal balance is key to preventing constipation.
Under stress, the body increases the production of cortisol, a hormone known to slow digestion and cause constipation. Chronically elevated cortisol levels can lead to long-term constipation.
When the body experiences stress, it naturally responds by releasing cortisol, known as the stress hormone. This hormone prepares the body to tackle the stressor by altering normal bodily functions, including digestion. It diverts energy and resources away from processes like digestion to areas needed for immediate response, such as the heart and muscles. This slowdown in digestive activity decreases gastrointestinal motility and the body’s ability to process food and eliminate waste efficiently, often resulting in constipation.
In normal situations, cortisol levels decrease once the stressor is removed. However, with chronic stress, these levels can remain persistently high, slowing digestion and leading to prolonged constipation.
This condition also dramatically affects the balance of gut bacteria, an essential factor for healthy bowel movements
3. Changes in Gut Microbiome
The gut microbiota, also known as gut flora, have a vital role in maintaining health. Stress can disturb the balance of bacteria in the gut, leading to dysbiosis – a condition that occurs when harmful bacteria outnumber beneficial ones. This imbalance can affect gut motility, leading to symptoms such as constipation. Furthermore, changes in gut microbiota can also affect the immune system and increase inflammation levels in the gut, leading to exacerbate digestive issues.
Slowing down transit resulted in a decrease in the fermentation efficiency of complex carbohydrates and a reduction in the production of short-chain fatty acids (SCFAs), including acetic acid, propionic acid, and butyric acid.
Butyric acid serves as an energy source for colonocytes and the host.
4. Inflammation, stress, and constipation
The gut, often referred to as the “second brain,” is sensitive to the effects of stress.
Continuing stress can lead to inflammation in the gastrointestinal tract, resulting in a disruption of normal bowel movements.
5 Why does stress cause constipation?
Depression, Anxiety and constipation
Psychiatric disorders, like depression, can be linked to constipation either because of the disease itself or other related factors. People with depression and other psychiatric disorders usually have unhealthy habits, like a bad diet, and reduced fluid intake. Furthermore, high-stress levels often result in poor sleep hygiene and physical inactivity, both of which contribute to constipation.
How do you treat stress-induced constipation?
Depression is linked to increased activity in the CRF neuronal pathways, and CRF receptors have been proposed as potential targets for treating depression and GI disorders. The activation of the stress pathways mentioned above may contribute to dysfunction in the brain-gut axis, rendering depressed patients more vulnerable to symptoms like chronic diarrhea or chronic constipation.
How to Reduce Stress-Related Constipation

- Comprehensive Constipation Management: Effectively managing stress-related constipation often requires a comprehensive approach that addresses both the physical symptoms and the underlying stress. Adopting dietary changes, engaging in regular physical exercise, utilizing stress management techniques, and incorporating natural remedies can all contribute to more effective management of constipation. This comprehensive approach ensures that the issue is tackled from various angles, increasing the likelihood of long-term relief and overall health improvement.
- Biofeedback therapy. Biofeedback is an amazing mind-body technique that empowers individuals to modify their physiology for better physical, mental, emotional, and spiritual health. Just like physical therapy, biofeedback training requires active participation and regular practice for optimal results. Clinical biofeedback can help manage symptoms and enhance overall health and wellness through stress management training.
- Stress Management Techniques: Managing stress levels has a vital role in soothing stress-related constipation. Regular physical activity, like yoga or walking, helps regulate cortisol levels and stimulate bowel movements. Incorporating mindfulness techniques, such as meditation or deep-breathing exercises, can also foster a sense of calm, reducing stress, and consequently, its impact on digestion.
- Cognitive Behavioral Therapy (CBT) is another effective stress management technique. It can help you understand and change thought patterns leading to stress, thereby improving digestion.
- Regular Exercise: Physical activities can stimulate the natural contraction of intestinal muscles, aiding in bowel movements. Moreover, exercise can also lower stress levels.
- Balanced Diet: Consuming a high-fiber diet can add bulk to the stool, making it easier to pass. Also, staying hydrated keeps the stool soft, preventing constipation. Include fenugreek in your diet, however not more than two teaspoons at a time, as any more may cause abdominal distress.
- Adequate Sleep: Sleep plays a vital role in the body’s natural stress response, and impacts weight and eating habits. Ensuring sufficient and quality sleep can help manage stress levels, thereby improving gut health.
- Herbal medicine: If you feel tense and “clench up”, relaxing nervine herbs such as vervain or chamomile are best. Aloe vera. Irritant laxatives, such as senna or cascara are sometimes used for constipation, but these can be harsh- they “irritate” the gut, causing expulsion. If used frequently the body can become reliant on them and may find it hard to “go” without them.
- Medication: In some cases, laxatives or stool softeners may be necessary. Always seek advice from a healthcare provider before using these medications.
Don’t let health concerns linger—empower yourself with knowledge and take control of your well-being. We’re here to help you!
What simple trick empties your bowels?
Stimulate proper digestion with bitters before eating; gentle demulcent herbs that help the stools to retain more water, softening and lubricating the bowels.
Demulcent herbs and seeds include psyllium husks, flaxseeds slippery elm, marshmallow root, and even porridge oats- they contain “gloopy “mucilages that hold water and make things “slippery”.
Use them as powders, add cold water, and allow them to sit until they are gloopy, and then drink them down.
Make sure that you get plenty of water- at least eight full glasses a day- to keep all that bulk moving through your digestive system
What are the side-effects of bulk-forming laxatives?
When you start using a bulk-forming laxative, you might experience some initial discomfort and abdominal distension. However, with continued use, these effects typically lessen, especially if you begin with a low dose and gradually increase it. Another option for patients dealing with significant bloating is methylcellulose, an inorganic bulking agent that doesn’t ferment. It’s important to note that rare cases of side effects, such as obstruction of the esophagus or colon, have been reported.
Do you have Asthma?
Do not take psyllium (Plantago ovata). There have been several reports of allergic reactions to psyllium, including a few serious asthma attacks from inhaled dust.
You should also watch how you react to this herb if you have allergies. If an allergic reaction occurs after you take it once, Do not use it again!
Conclusion
Stress hormones can trigger constipation by affecting gut motility and microbiota, as well as causing psychological issues that can interfere with normal bowel habits.
Maintaining cortisol levels within a healthy range is crucial for preventing stress-induced constipation.
By incorporating stress management techniques, making dietary modifications, engaging in regular exercise, and considering psychological interventions, individuals can address both stress and constipation to improve their overall well-being.
Disclaimer: This information is for educational purposes only and not a substitute for professional medical advice. It is also vital to consult healthcare professionals if symptoms persist to prevent further complications and receive personalized treatment plans.


[…] The 5 Interesting Hidden Links Between Stress and Constipation […]