Table of Contents
Struggling to lose weight despite eating well and exercising regularly?
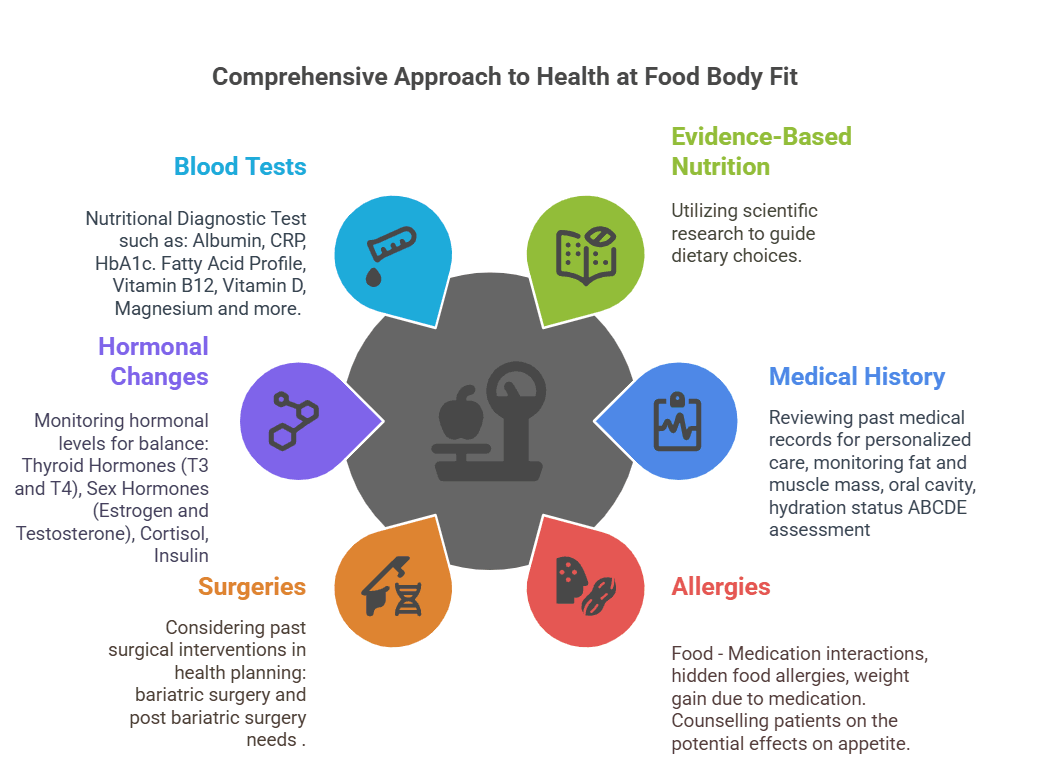
Can hormones affect weight loss?
Do you wonder how to reset female hormones for weight loss. You’re not alone. For many, the answer isn’t just calories in versus calories out—hormones could be the missing piece of your weight loss puzzle. From thyroid imbalances to insulin resistance, hormonal disruptions can sabotage metabolism, amplify cravings, and lock fat stores in place. In fact, research reveals that hormones like thyroid hormones (T3/T4), estrogen, testosterone, and growth hormone (GH) play pivotal roles in regulating body composition, energy expenditure, and even where fat is stored.
For instance, did you know that high baseline thyroid hormone levels may boost initial weight loss, but moderate dieting can reduce active T3, slowing metabolism? Or that sex hormone imbalances in obesity—like elevated estrogen in men or androgens in women—are linked to health risks such as breast cancer and low testosterone? Even growth hormone, which declines in obesity, can reshape abdominal fat distribution once restored. And let’s not forget insulin: this fat-storage hormone becomes a roadblock when cells grow resistant to its signals.
In this article, we’ll uncover the hormonal reasons for not losing weight, decode the signs of hormonal weight gain (think: stubborn belly fat, fatigue, or unexplained cravings), and explore science-backed strategies to rebalance your hormones for sustainable results. Whether you’re battling thyroid issues, PCOS, or metabolic slowdown, understanding your hormonal health could finally unlock your weight loss potential.
Keep reading to discover how your hormones might be holding you back—and how to reset female hormones for weight loss
Can hormones affect weight loss? Can hormones make it hard to lose weight?
Yes, hormones can absolutely make weight loss feel like an uphill battle. Beyond calorie counting and exercise, your endocrine system acts as a silent conductor of metabolism, fat storage, and hunger signals. When hormones like leptin, insulin, cortisol, or thyroid hormones fall out of balance, they can hijack your efforts, leading to unexplained weight gain, relentless cravings, and frustrating plateaus. Let’s dive into the clinical evidence and uncover how these hormonal disruptions work—and what you can do to reclaim control.
Hormonal Reasons for Not Losing Weight
1. Leptin Resistance: When Your Brain Ignores “Full” Signals
- Role: Leptin, produced by fat cells, signals the brain to suppress hunger and burn calories.
- Problem: In obesity, leptin levels rise, but the brain becomes resistant to its signals. This “leptin resistance” tricks the body into starvation mode, slowing metabolism and increasing appetite (Myers et al., 2012)1.
- Clinical Insight: Leptin resistance is linked to inflammation and high triglycerides, creating a vicious cycle of overeating (Crujeiras et al., 2010).
2. Insulin: The Fat-Storage Gatekeeper
- Role: Insulin regulates blood sugar by shuttling glucose into cells.
- Problem: Insulin resistance (common in obesity and PCOS) causes excess glucose to be stored as fat, particularly around the abdomen. High insulin levels also block fat breakdown (Kahn, 2012).
- Clinical Recommendation: Low-glycemic diets and intermittent fasting improve insulin sensitivity (Patterson et al., 2017).
3. Cortisol: The Stress-Induced Belly Fat Hormone
- Role: Cortisol mobilizes energy during stress.
- Problem: Chronic stress elevates cortisol, driving visceral fat deposition and cravings for sugary, high-fat foods (Epel et al., 2001).
- Sign to Watch: Weight gain concentrated in the abdomen, paired with fatigue and sleep issues.
4. Thyroid Hormones: Your Metabolic Thermostat
- Role: T3 and T4 regulate basal metabolic rate (BMR).
- Problem: Hypothyroidism (low T3/T4) slows metabolism, causing weight gain, cold intolerance, and fatigue. Even subclinical cases (TSH >4.5 mIU/L) reduce energy expenditure (Garber et al., 2012).
5. Sex Hormones: Estrogen, Testosterone, and Stubborn Fat
- Estrogen Dominance: Excess estrogen (or low progesterone) in women promotes fat storage in hips/thighs. Men with obesity often have low testosterone and elevated estrogen, worsening abdominal fat (Lizcano & Guzmán, 2014).
- PCOS Link: High androgens (e.g., testosterone) in women drive insulin resistance and weight gain (Barber et al., 2019).

Growth Hormone (GH) Deficiency: Low GH reduces muscle mass and increases fat accumulation, particularly in adults over 40
Want a personalized approach? Work with a clinical nutritionist today!
Signs of Hormonal Weight Gain: What Your Body Is Telling You
Example: Rapidly gaining 5–10 lbs without changes to diet or exercise.
Hormonal Culprits:
- Hypothyroidism: Low thyroid hormones (T3/T4) slow metabolism, reducing energy expenditure by up to 15–40%
- Insulin Resistance: Excess insulin promotes fat storage and inhibits lipolysis (fat breakdown)
- Cortisol Dysregulation: Chronic stress raises cortisol, which increases visceral fat deposition
- Leptin Resistance: Despite high leptin levels, the brain ignores “full” signals, driving overeating
- Growth Hormone (GH) Deficiency: Low GH reduces muscle mass and increases fat accumulation, particularly in adults over 40 (Veldhuis et al., 2005).
According to Garber et al., 2012, women with untreated hypothyroidism gained an average of 5–10 lbs within 6 months, even with calorie restriction.
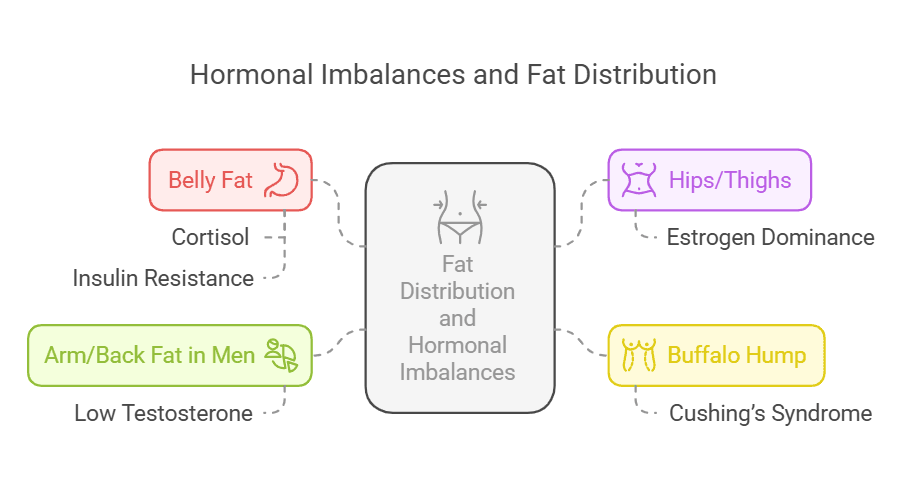
2. Fat Distribution Shifts
Where your body stores fat often reflects hormonal imbalances:
- Belly Fat (Visceral Adiposity):
- Cortisol: Stimulates fat storage around organs
- Insulin Resistance: Promotes lipogenesis in abdominal fat cells
- Hips/Thighs (Subcutaneous Fat):
- Estrogen Dominance: Directs fat to lower body areas; common in perimenopause
- “Buffalo Hump” (Upper Back/Neck Fat):
- Cushing’s Syndrome: Excess cortisol from adrenal tumors or prolonged steroid use
- Arm/Back Fat in Men:
- Low Testosterone: Reduces muscle mass, increasing fat retention in atypical areas
Visceral fat releases inflammatory cytokines (e.g., IL-6) that worsen insulin resistance, creating a feedback loop (Tchernof et al., 2013).
Struggling with Menopause Belly Fat? Here’s the Solution!
Nuciferine, a powerful alkaloid from the lotus leaf (Nelumbo nucifera), is gaining attention for its fat-burning and hormone-balancing benefits.
✅ Supports Fat Metabolism – Activates fat-burning pathways to reduce stubborn weight
✅ Balances Hormones – Helps regulate dopamine and insulin for better metabolic control
✅ Reduces Inflammation – Combats oxidative stress that leads to belly fat storage
✅ Supports Insulin Sensitivity – Helps prevent fat accumulation linked to hormonal changes
3. Mood Swings and Fatigue
Hormones heavily influence mental health and energy levels:
- Thyroid Hormones: Hypothyroidism is linked to depression, brain fog, and fatigue due to reduced cerebral blood flow.
- Serotonin Imbalance: Low estrogen (e.g., menopause) reduces serotonin synthesis, increasing irritability and cravings .
- Cortisol: Chronic elevation depletes dopamine, worsening mood swings
- Progesterone: Sharp drops (e.g., PMS, perimenopause) reduce GABA activity, heightening anxiety
Actionable Fix:
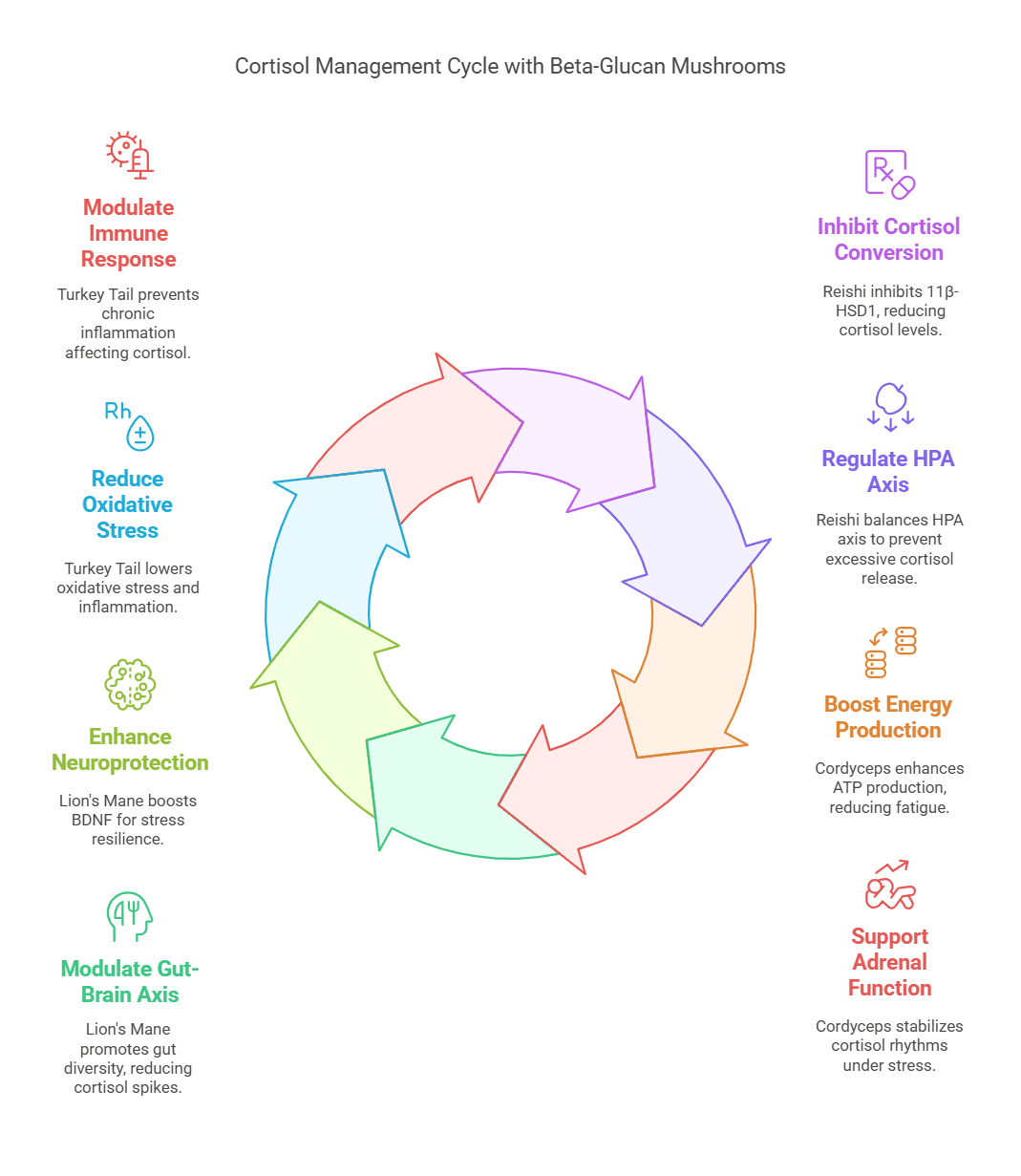
- Beta-Glucan Mushrooms: Incorporate adaptogenic mushrooms like Reishi, Cordyceps, and Lion’s Mane to support hormonal balance:
- Why Beta-Glucans?
- Beta-glucans in these mushrooms act as:
- Immune Modulators: Reduce systemic inflammation driving insulin and leptin resistance (Jayachandran et al., 2017).
- Prebiotics: Feed gut bacteria that produce serotonin (95% of which is made in the gut), indirectly improving mood and satiety (Bashir & Choi, 2017).
- A 2020 study found that Reishi extract (1.5g/day) lowered cortisol by 24% and improved sleep quality in stressed adults, indirectly supporting weight loss (Liao et al., 2020).
- Omega-3 fatty acids (2g/day EPA/DHA) improve serotonin function and reduce cortisol
Order now supplements for hormonal weight gain
4. Irregular Periods or PCOS Symptoms
- High Androgens (Testosterone): Disrupt ovulation, causing irregular cycles and acne. Androgens also increase visceral fat via insulin resistance (Barber et al., 2019).
- Anti-Müllerian Hormone (AMH): Elevated AMH in PCOS correlates with ovarian dysfunction and weight gain (Dewailly et al., 2016).
- Low Sex Hormone-Binding Globulin (SHBG): Common in PCOS, leading to higher free testosterone and estrogen (Goodman et al., 2015).
PCOS & Weight Link: Women with PCOS have 3x higher risk of abdominal obesity compared to controls (Lim et al., 2019).
5. Additional Signs of Hormonal Imbalance
- Night Sweats/Hot Flashes: Fluctuating estrogen disrupts hypothalamic temperature regulation (Freedman et al., 2002).
- Hair Loss or Hirsutism:
- Low Thyroid Hormones: Thinning hair (Vincent et al., 2013).
- High Androgens: Facial/body hair growth (Azziz et al., 2000).
- Carbohydrate Cravings:
- Leptin Resistance: Compulsive snacking due to poor satiety signaling
- Ghrelin Surges: Stress-induced ghrelin spikes drive sugar cravings
Evidence-Based Solutions to Rebalance Hormones
- For Insulin Resistance:
- Berberine: 500mg 3x/day improves insulin sensitivity comparably to metformin (Zhang et al., 2010).
- For Estrogen Dominance:
- DIM (Diindolylmethane): 200mg/day supports healthy estrogen metabolism (Thomson et al., 2016).
- For Cortisol Management:
- Beta-Glucan Mushrooms as Adaptogens for Cortisol Management
- Reishi (Ganoderma lucidum) Dose: 1.5–3g/day of dual-extracted powder.
- Cordyceps (Cordyceps militaris) 1–3g/day of fruiting body extract
- Boosts ATP Production: Enhances mitochondrial energy output, reducing fatigue and lowering cortisol’s catabolic effects on muscle
- Supports Adrenal Function: Increases resilience to physical and emotional stress, stabilizing cortisol rhythms.
- Lion’s Mane (Hericium Herinaceus) 3–5g/day of powdered extract.
- Gut-Brain Axis Modulation: Beta-glucans in Lion’s Mane promote gut microbiota diversity, reducing inflammation-driven cortisol spikes
- Neuroprotection: Enhances BDNF (brain-derived neurotrophic factor), improving stress resilience and mood stability
- Turkey Tail (Trametes versicolor) Dose: 3–6g/day of hot water extract
- Polysaccharide-K (PSK): Reduces oxidative stress and inflammation, indirectly lowering cortisol’s impact on fat storage (Standish et al., 2008).
- Immune Modulation: Beta-glucans regulate immune responses, preventing chronic inflammation that exacerbates cortisol dysregulation.
When to Test Your Hormones
- Comprehensive Panel: TSH, Free T3/T4, AM cortisol, DHEA-S, estradiol, progesterone, testosterone, fasting insulin, HbA1c.
- Specialized Tests: 24-hour urinary cortisol (for Cushing’s), AMH (for PCOS).
What hormones should I check when not losing weight?
1. Insulin
- Role: Regulates blood glucose and fat storage. Insulin resistance (common in obesity or PCOS) promotes fat accumulation, particularly visceral fat.
- Testing: Fasting insulin, glucose, HbA1c, and HOMA-IR (Homeostatic Model Assessment for Insulin Resistance).
2. Leptin
- Role: Signals satiety to the brain. Obesity often causes leptin resistance, blunting its effect and increasing hunger.
- Testing: Serum leptin (elevated in resistance). Note: Levels correlate with body fat.
3. Thyroid Hormones (TSH, Free T3, Free T4)
- Role: Regulate metabolic rate. Hypothyroidism (high TSH, low T3/T4) slows metabolism.
- Testing: TSH, free T3, free T4, and thyroid antibodies (anti-TPO) for autoimmune causes.
4. Cortisol
- Role: Chronic stress elevates cortisol, increasing abdominal fat and appetite via visceral fat deposition.
- Testing: Diurnal salivary cortisol (4x/day) or 24-hour urinary free cortisol.
5. Estrogen and Progesterone
- Role: Estrogen dominance (low progesterone relative to estrogen) or perimenopausal declines in estrogen can increase visceral fat and insulin resistance.
- Testing: Serum estradiol, progesterone (day 21 of cycle), FSH, LH.
6. Testosterone (Total and Free)
- Role: Low testosterone in women reduces lean muscle mass, lowering BMR. High testosterone (PCOS) drives insulin resistance.
- Testing: Total testosterone, free testosterone, SHBG.
7. Ghrelin
- Role: Stimulates hunger. Dysregulation occurs in obesity or poor sleep.
- Testing: Fasting ghrelin (limited clinical utility; focus on symptom management).
8. Anti-Müllerian Hormone (AMH) and Androgens (DHEA-S, Androstenedione)
- Role: Elevated in PCOS, contributing to insulin resistance and weight gain.
- Testing: AMH, DHEA-S, androstenedione.
9. Growth Hormone (GH) and IGF-1
- Role: GH stimulates lipolysis. Low IGF-1 (a GH marker) correlates with abdominal obesity.
- Testing: IGF-1 levels.
10. Prolactin
- Role: Elevated prolactin (hyperprolactinemia) disrupts estrogen/testosterone, increasing appetite.
- Testing: Serum prolactin.
Lifestyle Considerations
- Sleep: Poor sleep disrupts leptin/ghrelin (Taheri et al., 2004).
- Stress Management: Meditation/yoga lowers cortisol (Pascoe et al., 2017).
- Diet: Fiber-rich, low-glycemic diets improve insulin sensitivity (Ludwig, 2002).
Clinical Recommendations
- Consult an endocrinologist or nutritionist for personalized testing.
- Address insulin resistance via low-glycemic diets, resistance training, and metformin if indicated.
- Optimize thyroid function with selenium/zinc
- Manage cortisol with stress reduction and adaptogens (e.g., beta glucan).
Note: Always interpret labs in context with symptoms and clinical history. Hormonal interactions are complex; a systems-based approach is essential.
How to Stop Hormonal Weight Gain: Evidence-Based Strategies
- Balance Blood Sugar
- Eat Protein/Fiber First: Reduces insulin spikes by 40% (Shukla et al., 2019).
- Try Time-Restricted Eating: 12–14-hour fasting windows improve insulin sensitivity.
- Lower Cortisol Naturally
- Adaptogens: Beta Glucan Mushrooms, Ashwagandha reduces cortisol by 28% in chronic stress
- Sleep Hygiene: Aim for 7–9 hours; poor sleep raises cortisol and ghrelin (hunger hormone).
- Support Thyroid Function
- Selenium & Zinc: Critical for T4-to-T3 conversion
- Avoid Goitrogens: Limit raw cruciferous veggies (e.g., kale) if hypothyroid.
- Target Estrogen Balance
- Fiber-Rich Diet: Flushes excess estrogen via gut detoxification
- DIM Supplements: Diindolylmethane (from broccoli) supports healthy estrogen metabolism.
When to Test Your Hormones
Consult a healthcare provider if you experience:
- Unexplained weight gain + fatigue.
- Persistent cravings or irregular periods.
- Family history of thyroid disease or PCOS.
Key Tests: TSH, Free T3/T4, fasting insulin, cortisol (salivary), estrogen, testosterone.
Conclusion
Hormones are powerful regulators of weight—but they’re not destiny. By addressing insulin resistance, stress, thyroid health, and estrogen balance, you can reset your metabolism and finally break through plateaus. Always pair lifestyle changes with professional guidance for personalized care.
- Challenges and Opportunities of Defining Clinical Leptin Resistance
Myers, Martin G. et al. Cell Metabolism, Volume 15, Issue 2, 150 – 156 ↩︎


[…] Can hormones affect weight loss? Hormonal reasons for not losing weight […]